surgical techniques
Snapping scapula
Definition
Disruption of the normal smooth motion of the scapulothoracic joint
- posterior scapula pain with overhead motion
Etiology
1. Bony abnormalities
- osteochondromas
- prominence of the superior medial border of the scapula / Luschka tubercle
2. Soft tissue abnormalities
- bursitis / scar tissue
- muscular weakness
3. Masses
Femoral Head Fractures
Incidence
5-15% of posterior dislocations
Aetiology
Posterior hip dislocation
Pipkin Classification
Type I - head fracture below fovea
Undisplaced
- non operative
Displaced
- excise fragment if small
- ORIF fragment if large (can contribute to instability)
Subtalar and Triple Arthodesis
Biomechanics
Able to achieve relatively high level of function after STJ fusion
- previously believed that isolated STJ fusion should not be performed
- believed that triple arthrodesis was operation of choice for hindfoot
- STJ fusion has superior result with less stress on AJ
Average loss of DF 30% / PF 10%
Position of hindfoot determines flexibility of transverse tarsal (CCJ & TNJ) joints
- imperative that fusion be positioned in ~ 5o valgus
Radial head fractures
Radial Head Fracture
Mechanism
FOOSH
- axial load with a valgus force
Biomechanics
1. Provides Valgus stability
- especially if MCL deficient
2. Longitudinal stability
- aided by interosseous membrane
3. Load Transfer
- 60% of load at elbow
DDH
Concept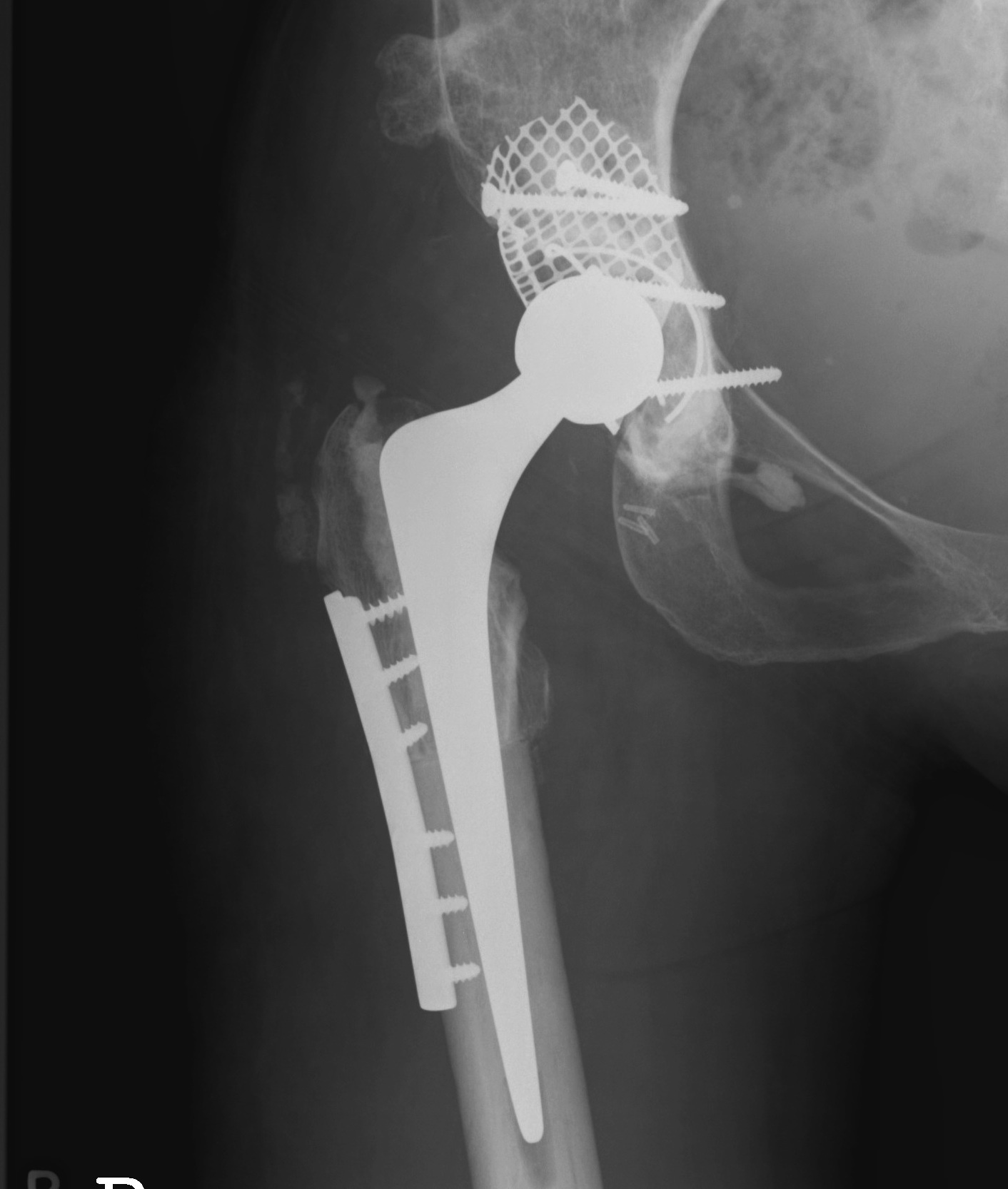
THR in dysplastic hips has a higher failure rate
- due to anatomic abnormalities
- due to generally younger age
Aim
Restore normal biomechanics and preserve bone stock
Issues
Soft tissues
Chronic lateral ankle instability
Definition
Chronic instability due to rupture of one or more parts of the lateral ligament
Anatomy
Progressive injury
1. Anterolateral capsule
2. ATFL
3. CFL
NHx
Can lead to ankle OA over time

