
Epidemiology
Much less common than hip and knee OA
Patients tend to be younger
Etiology
Primary ankle OA is uncommon, 80% of ankle OA is post-traumatic
- 406 patients with end stage ankle OA
- 80% post-traumatic
- 13% secondary OA
- 9% primary OA
Trauma
| Ankle Fracture | Plafond Fracture | Talus | Ligament Instability |
|---|---|---|---|
|
Swierstra et al EFORT Open Rev 2022 - systematic review ankle fractures - 25% OA |
Harris et al Foot Ankle Int 2006 - 79 tibial plafond ORIF - 2 year follow up - 40% OA |
Talus osteochondral lesions Talus malunion / AVN post neck fracture |
Lofenberg et al Foot Ankle Int 1994 - 37 patients with chronic ankle instability - 20 year follow up 13% OA |
 |
 |
 |
 |
Secondary OA
Rheumatoid OA / Inflammatory OA / Infection / Hemochromatosis / Hemophilia / Charcot
Anatomy
Thin cartilage 1 mm
Joint highly congruent
- 1mm shift causes 40% decrease in contact area
- increases tibio-talar contact stresses
Clinically
Pain
- with weight bearing
- nightime
Stiff ankle joint
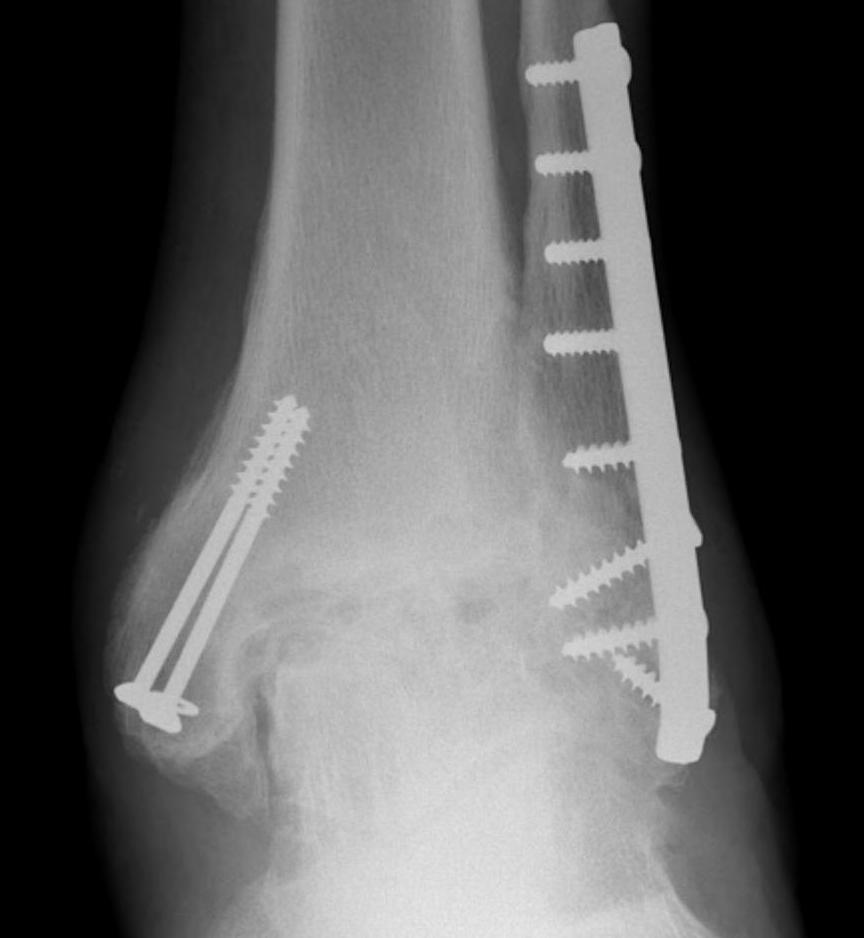
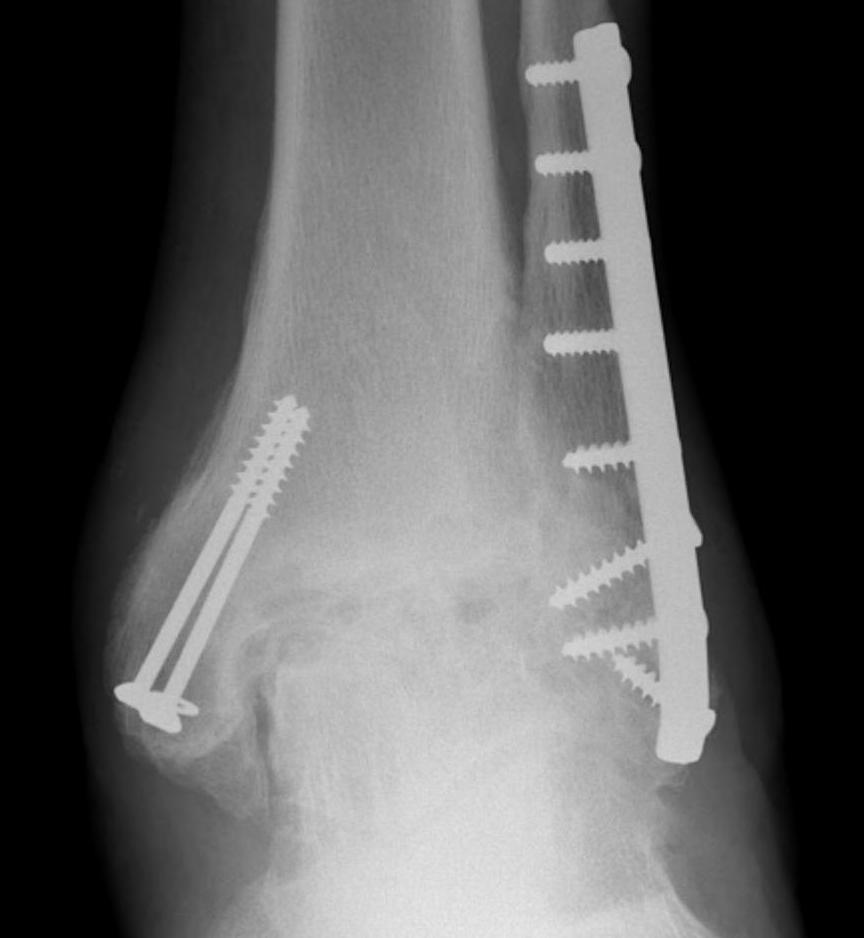
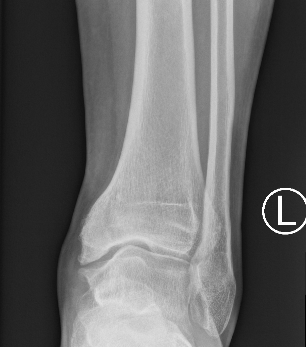
Xray
Ranges from anterior spurring to severe OA
80% of post-traumatic OA is varus
Takakura classification
| Grade | Description |
|---|---|
| 1 | Early sclerosis and formation of osteophytes |
| 2 | Narrowing of the medial joint space |
| 3A | Obliteration of the medial joint space with subcondral bone contact |
| 3B | Obliteration of joint space over roof of talar dome, with subchondral bone contact |
| 4 | Obliteration of joint space with complete tibiotalar contact |

Type 1: Anterior spurs


Type 3A: Obliteration of medial joint space Type 3B: Obliteration medial joint space plus tibio-talar contact with varus


Type 4 complete obliteration
CT

Small anterior tibial spur


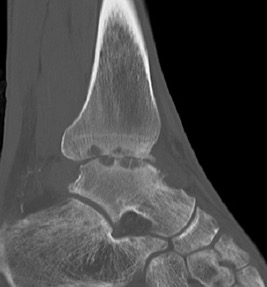
Large cysts in patient with ankle OA
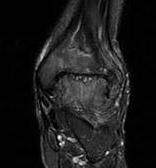
MRI


Management
Non Operative
PRP
- systematic review of 4 studies using PRP for ankle OA
- evidence of improved pain and function at 6 months
Hyaluronic acid
Vannbouathong et al Foot Ankle Int 2018
- systematic review of HA for ankle OA
- 3 RCTs
- evidence for improved pain with HA versus saline at 6 months
Operative
Options
Arthroscopy
Ankle distraction arthroplasty / arthrodiastasis
Arthrodesis
Supramalleolar osteotomy
Arthroplasty
Arthroscopic debridement
Indication
Anterior impingement
- kissing osteophytes on anterior tibia and talar neck
www.boneschool.com/footandankle/anteriorimpingement
Ankle distraction arthroplasty / arthrodiastasis
Theory
Allows some cartilage regeneration and healing
Young patient
Technique
Vumedi ankle distraction arthroplasty
Hinged external fixation distracting joint
- 3 - 4 months
- distracted 5 mm
Results
Arshad et al Foot Ankle Surg 2022
- systematic review distraction arthroplasty
- most improvement at or slightly above MCID (minimal clinically important difference)
- 50% revision to arthrodesis or arthroplasty
Supramalleolar Osteotomy


Varus OA treated with medial opening wedge supramalleolar osteotomy
Indications
Varus / valgus malalignment
Asymmetric OA with preserved cartilage in 50% of ankle (Grade 2 and 3A)
Technique
Surgical technique supramalleolar osteotomy PDF
Surgical technique supramalleolar osteotomy video
Results
- systematic review of 24 studies and 1200 patients
- failure rate 7%
- complication rate 5%
- nonunion rate 2%
Arthrodesis versus Arthroplasty
Functional outcome
Shih et al Foot Ankle Surg 2020
- meta-analysis arthrodesis v arthroplasty last 10 years (3rd generation ankle arthroplasty)
- no difference in total outcome scores / pain / gait / satisfaction between two groups
- improved function and ROM with arthroplasty
- higher complication and reoperation with arthroplasty
- meta-analysis of 37 studies comparing arthrodesis and arthroplasty
- Arthroplasty PROMs > arthrodesis in the short term (<2y)
- Arthroplasty PROMs = arthrodesis in the medium term (2-5y)
- Arthrodesis PROMs > arthroplasty in the long term (>5y)
Revision rate
- database of ankle fusions v arthroplasty
- 5 year subtalar arthrodesis rate: ankle fusion 3%
- 5 year subtalar arthrodesis rate: arthroplasty 0.7%
Subtalar arthritis
- database of ankle fusions v arthroplasty
- 5 year subtalar arthrodesis rate: ankle fusion 3%
- 5 year subtalar arthrodesis rate: arthroplasty 0.7%
Ankle Arthrodesis
www.boneschool.com/footandankle/anklearthrodesis
Ankle Arthroplasty
http://www.boneschool.com/lower-limb/foot-and-ankle/ankle-arthroplasty
