Mechanism
FOOSH
Epidemiology
Age 6 as maximum ligamentous laxity
- < 4 - physeal separation
- > 8 - dislocation
Male > F
2nd most common upper limb fracture in children (after distal radius)
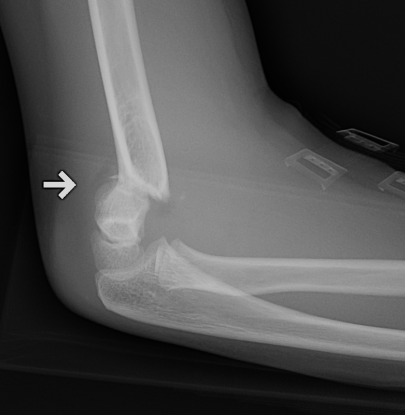
Pathoanatomy
Supracondylar region in 6 year old is thin
- thinnest at olecranon fossa (2-3 mm)
- thin lateral & medial columns
Children also tend to hyperextend at the elbows due to increased ligamentous laxity
With increasing hyperextension, the anterior periosteum hinge is torn
Examination

Clinical
"S" Shaped arm which is very swollen
Pucker sign
- anterior spike impales brachialis to skin

Nerve examination
1. Median nerve
- sensation
2. Anterior interosseous nerve (AIN)
- make circle with index and thumb
- check FPL and FDP index finger
- most common injury in extension type fractures
3. Posterior interosseous nerve (PIN)
- thumb up
4. Ulna nerve
- cross fingers / spread fingers / sensation
- most common injury in flexion type fractures
5. Radial nerve
- decreased sensation first dorsal webspace
Classifications
Flexion type 2%

Extension type 98%
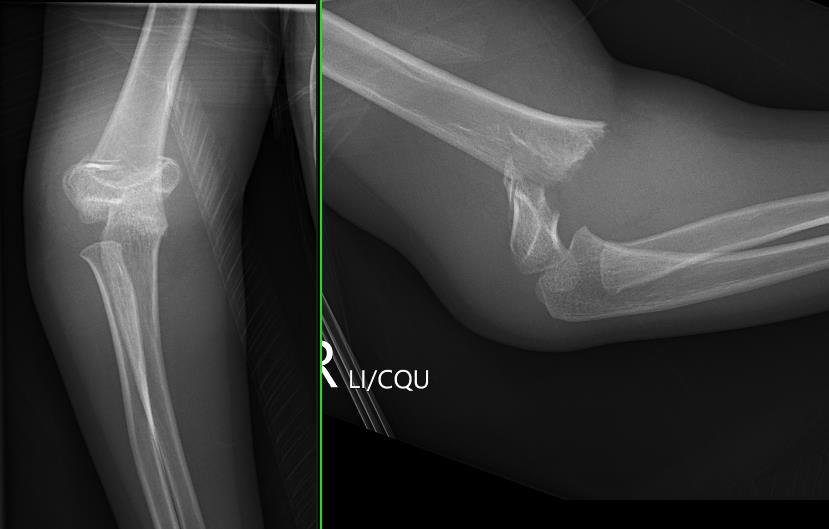
Gartland Classification Extension Fractures
Gartland I - Undisplaced
- < 2 mm
- anterior and posterior cortices intact

Gartland II - Displaced with intact posterior cortex
- > 2 mm
- anterior humeral line passess anterior to capitellum
- posterior periosteum is intact
Gartland III - Displaced, nil cortical contact
- completely displaced
- posteromedial or posterolateral

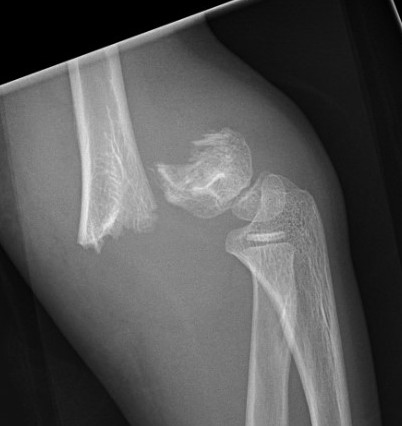
Gartland IV - Nil cortical contact with complete periosteal disruption
Extremely unstable at surgery in both flexion and extension planes
Modified by Wilkins
Type IIB Rotated


Type IIIA Posteromedial
Commonest
- distal fragment goes posteromedial
- cause cubitus varus
- injures radial nerve which is tethered over lateral spike on proximal fragment
- manage by pronation which tightens medial periosteal hinge
Type IIIB Posterolateral
Distal fragment goes posterolateral
- causes cubitus valgus
- tend to ER
- injuries median nerve & brachial artery
- these get tethered over medial spike on proximal fragment
- manage by supination which tightens lateral periosteal hinge
The position of stability is achieved with the thumb pointed towards the side of the periosteal disruption
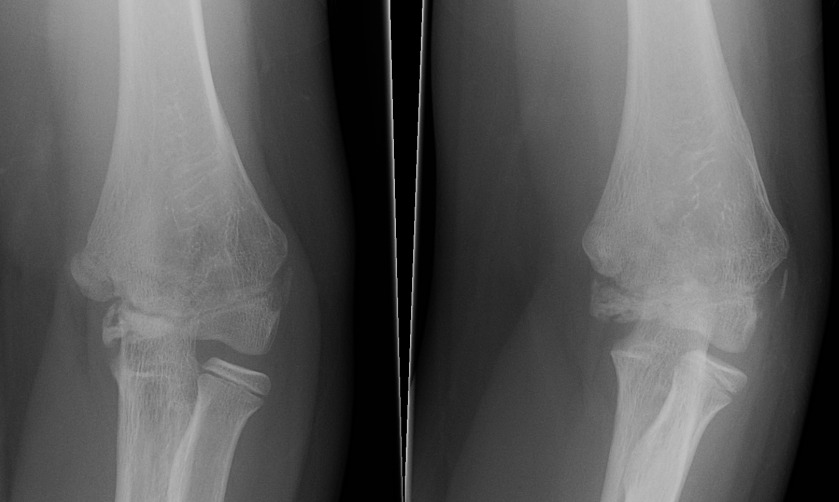
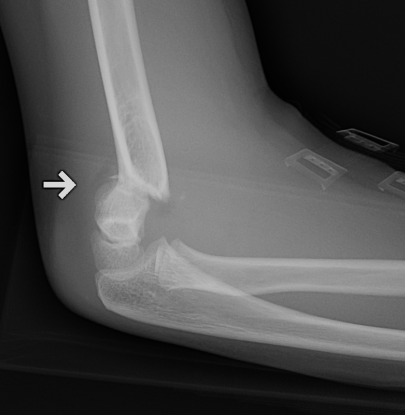
Lateral Xray
Position for good lateral
- thumb vertical
- hand above elbow
Anterior angulation
- shaft - condylar axis
- normally 40o
Lines


Anterior humeral line (AHL)
- should pass through middle of capitellum
Radio-capitellar line
- pass through capitellum
Teardrop
- shadow above the capitellum
- anterior dense line: posterior margin of the coronoid fossa
- posterior dense line: anterior margin of the olecranon fossa
- inferior portion: ossification center of the capitellum
AP X-ray
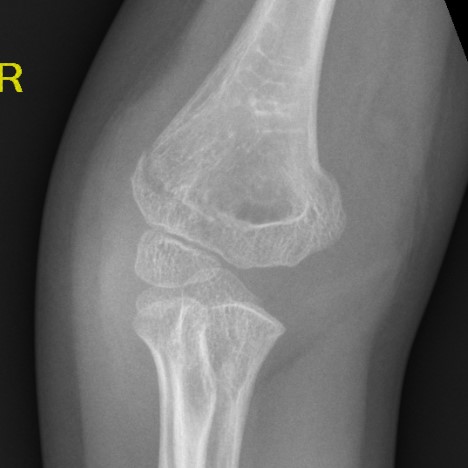
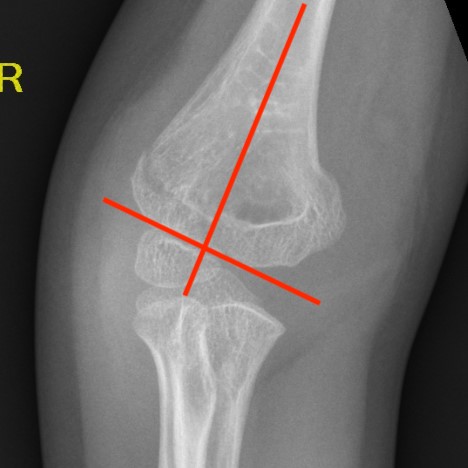
Baumann's Angle
Technique
- angle between longitudinal axis humerus and capitellar physis
- should equal uninjured side
- 75o normal
Cubitus varus
- varus malposition > 81°
Cubitus valgus
- < 70o
Management
Free review articles
Vaquero-Picado et al, EFORT OR 2018
Issue
There is limited remodelling potential of the distal elbow after the age of 4
After age 8 - 10, only 10% of growth of humerus remains
Algorithm
Type 1
Cast / collar and cuff
- flex up to splint with triceps
- 3/52
Type 2A
Closed reduction
- anterior humeral line doesn't contact capitellum
- Baumann's angle > 800 (cubitus varus)
- immobilise in flexion
- careful watching for late displacement
Ojeaga et al. J Paediatr Orthop 2020
- 77 type IIa patients
- 77% successfully treated with closed reduction and cast
Roberts et al. J Paediatr Orthop 2018
- compared collar and cuff / flexion taping with cast in 39 patients
- no difference
Type 2B
By definition, have rotation
- MUA + K wire
Type III
MUA + K wire
Flexion type
Timing of surgery
Takeaway message
- earlier surgery is probably technically easier due to swelling
- surgery can be difficult
- don't do in the middle of the night unless emergency / vascular compromise
- systematic review of 5 non randomized retrospective studies
- 396 patients
- increased failure of closed reduction with conversion to open reduction with surgery performed > 12 hours
Farrow et al. Bone Joint J 2018
- meta-analysis showed no difference between early and delayed surgery
Pauci et al. J Orthop Trauma 2018
- increased incidence malunion in surgery performed after midnight
- fractures treated after midnight tended to be more severe
Surgical technique
Options
- lateral K wires
- crossed K wires
- systematic review and meta-analysis
- 11 studies (RCTs and prospective cohorts)
- 1158 patients
- loss of reduction in 11.6% of crossed K wires and 12.4% of lateral K wires
- iatrogenic ulna nerve injury in 4% crossed K wires and 0.3% lateral K wires
Carrazzone et al. J Should Elbow Surg 2021
- meta-analysis of 12 RCTs
- no difference in functional outcome
- reduced risk of iatrogenic nerve injury with lateral K wires
- greater fixation stability and less loss of reduction with crossed K wires
Closed reduction and K wire technique
Set up
On arm table
Sterile tourniquet available should open reduction be required
Manipulation technique (must have adequate reduction, or very unstable and cannot K wire)
1. Consider milking any soft tissues that may be trapped (pucker sign)
2. In-line traction at 30o
- 2 minutes to overcome soft tissues
- check fluoroscopy
3. Reduce translation / rotation / varus and valgus
- adjust carrying angle / Baumann's angle
- avoid medial impaction / cubitus varus
- supination - maximise the traction on the lateral ligments to disimpact lateral side
- pronation - maximise traction on the medial ligaments to disimpact medial side
- check fluoroscopy
4. Flexion pushing olecranon forward with thumb
- shoot through AP to assess reduction
- check Baumann's angle
- check medial and lateral columns with oblique views
5. Hand position (point thumb towards side of impaction)
- posteromedial displacement - hyperpronation in flexion
- posterolateral displacement - hypersupination in flexion
6. Check lateral image
- lock elbow in flexion and rotation
- externally rotate the shoulder
- ensure that the anterior humeral line is correct
- reduction of teardrop on lateral
- may need to increase the flexion
Bony landmarks
In extension
- medial / lateral epicondyle and olecranon all in a line
In flexion
- medial / lateral epicondyle with olecranon from equilateral triangle
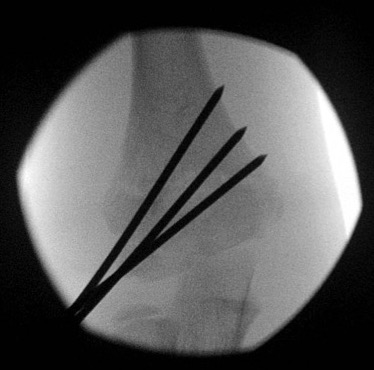
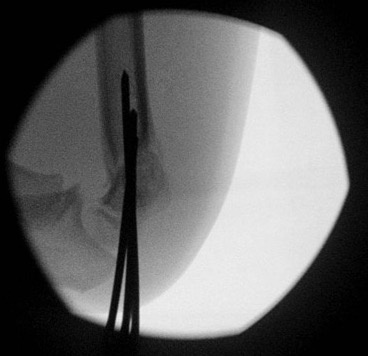
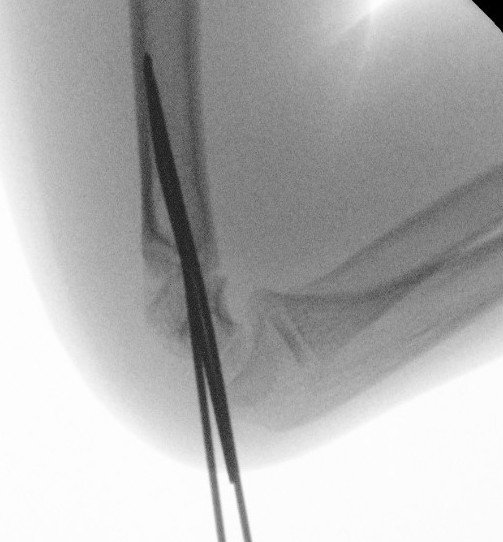
2 x lateral K wires
Advantage
- no risk to ulna nerve
Disadvantage
- if not correctly done, can be unstable
Technique
- hold elbow in flexion
- place K wire into lateral condyle
- place other index finger on the humerus to guide aim
- 2 x lateral 1.6 mm K wires (consider 2 mm K wires in larger children)
- one K wire on the direct lateral surface, just lateral to the capitellum
- one on the capitellar surface
Points
- must engage medial and lateral columns (bicortical)
- make pins divergent for increased stability
- only need 3rd pin if first two not divergent enough
Check stability
- place elbow into extension
2. Crossed K wires 1.6mm

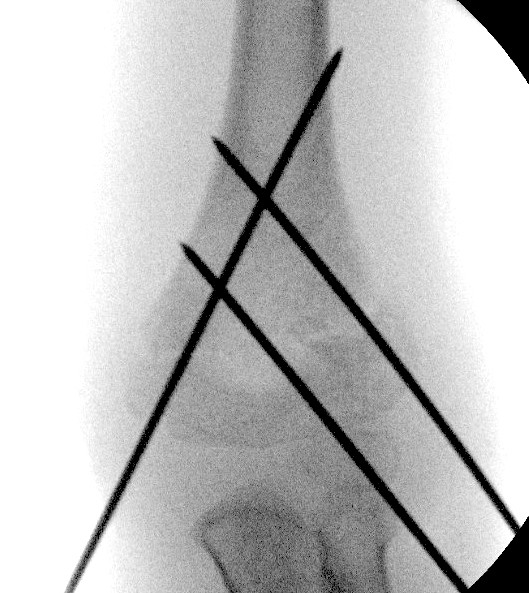
Advantage
- increased biomechanical strength
- maybe necessary with signification medial comminution
- maybe necessary if unstable after two lateral K wires
Disadvantage
- ulnar nerve at risk
Small medial open approach
- place arm in external rotation
- place local anaesthetic with adrenaline to decrease bleeding (tourniquet not typically needed)
- mini open approach over medial epicondyle
- dissect down onto the hard medial epicondyle
- identify the common flexor origin to confirm
- K wire directly onto bone
- may need to extend elbow to 90o as in some children the ulna nerve subluxes anteriorly in flexion
- K wire must aim posterior to anterior as medial epicondyle is posterior
Points
- wires must cross above the level of the fracture
- engage medial and lateral cortices
3. Technical issues
1. Significant medial comminution
- cross K wires
2. Unstable with excessive flexion
- cross table lateral
- place bump under humerus
- reduce flexion
- may need cross K wires
3. Ipsilateral distal radius fracture
- MUA and K wire the distal radius first
Post operative
Check pulse (use doppler if needed)
Bend and leave K wires protruding
Cast
Remove K wires at 3 weeks
Irreducible supracondylar fracture
Problems
- brachialis might be trapped
- brachial artery might be in fracture
Management
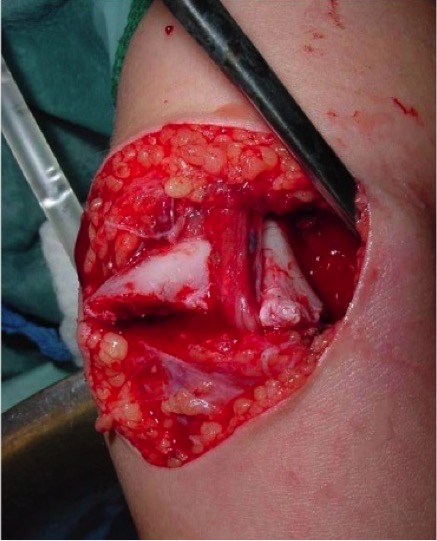
Sterile tourniquet
Anterior approach
- identify biceps tendon laterally
- identify and tag the median nerve medially
- identify and tag the brachial artery and two venae commitantes between biceps tendon and median nerve
- release soft tissue especially carefully release lacertus
- safest over the median nerve
- open and clean fracture spikes both medially and laterally
- remove any brachialis and periosteum that might block reduction
- perform open fracture reduction with finger
- flex arm and check flouroscopy
Pulseless supracondylar
Scenarios
1. Pulseless but pink and perfused on presentation
Make vascular surgeons aware
Urgent closed reduction + K wire
- position at 90o
- ensure pulse returns
- observe closely
- 42/60 patients had pulse return immediately after closed reduction and pinning
3. Pink and well perfused after reduction, no pulse
The pulse will return in virtually all patients
- some however on surgical exploration or doppler will be shown to have significant vascular injury
- pulse returns eventually due to collaterals
- patients typically do well regardless
Recommend close observation
- consider exploration if no waveform on pulse oximeter
- consider doppler ultrasound
- 1297 supracondylar fractures
- 20 with pink hand, doppler pulse but non palpable pulse after reduction
- all observed closely
- 19/20 pulse returned by discharge or by first post op visit
- 1/20 developed white hand 9 hours post surgery, and needed urgent vascular repair
- 18 patients with pink pulseless hands had a delayed pulse return up to 11 days later
- long term follow up on 20 patients with perfused pulseless hand after closed reduced
- all 20 had palpable pulse
- 5/20 had brachial artery occlusion with large collateral vessels on doppler ultrasound
- all patients had normal growth and excellent function
Soh et al. Clin Orthop Surg 2013
- 26 patients with pink and perfused
- pulse oximeter used
- 4/26 no waveform on pulse oximeter, all had vascular injury
- 22/26 had wave on pulse oximeter, pulse subsequently returned in all
Noaman et al. Microsurgery 2006
- 31 patients with no pulse explored
- all 31 had significant vascular findings including traumatic aneurysm and transection
2. Hand white, non perfused, no pulse on doppler after reduction
Surgical emergency
- vascular surgeon
- lazy S approach
- 1297 supracondylars
- 5 patients with white hand and no pulse
- all 5 underwent either primary repair or saphenous vein graft
4. Pulse present before surgery, no pulse & hand white after closed reduction
Brachial artery entrapped in fracture
- anterior lazy S approach
- expose and release brachial artery
- open reduction and K wire
Too swollen / skin abraded
1. Skin traction
- arm straight
- weight over pulley
- body weight counter traction
2. Dunlop traction
- screw in olecranon
- bent arm traction
- difficult to control rotation
Complications
Nerve Injury
Anterior interosseous nerve (AIN)
Most commonly injured
Indications for exploration
- post reduction nerve injury with non anatomical reduction
- open injury
- 35 cases of supracondylar fracture with isolated AIN injury
- all patients had complete return of AIN at mean 49 days (range, 2 - 224 days)
Median / ulna nerve / radial nerve
Ulna nerve
- associated with flexion type supracondylar fractures
- can be injured during medial K wire (avoid with mini-open approach)
Median nerve
- more often injured with severe fractures
- can be injured with lateral K wires
Compartment Syndrome
Extremely rare, case reports only
However, must monitor overnight as the results of missed acute compartment syndrome are devastating
- 4400 cases of operatively treated supracondylar fracture
- no patient development compartment syndrome
Volkmann's contractures
- permanent flexion of the wrist and hand
- caused by shortening of the flexor muscles of the forearm
Malunion
Issues
Sagittal plane deformity will remodel
Coronal plane deformity & rotation will not
Cubitus Varus




Most common deformity
- mainly cosmetic problem
- can also be due to medial growth arrest
Treatment


Oblique closing wedge osteotomy via lateral approach
JBJS Essential Surgical Techniques
Results
Solfelt et al. Bone Joint J 2014
- systematic review of 894 children treated for cubitus varus
- mean correction 27o
- 88% good or excellent results
- nerve palsy in 2.5%, although the majority were transient
- compared coronal plane osteotomy only with multiplane osteotomy
- 86 elbows with cubitus varus
- more loss of correction with multiplane osteotomy
Cubitus Valgus
Uncommon
- may cause tardy ulna nerve palsy
- manage by transposing nerve

Stiffness
Myositis ossificans uncommon
- may be secondary to remanipulation > 1/52 / later presentation
Stiffness usually minimal
- takes up to 1 year to regain full motion
- especially extension
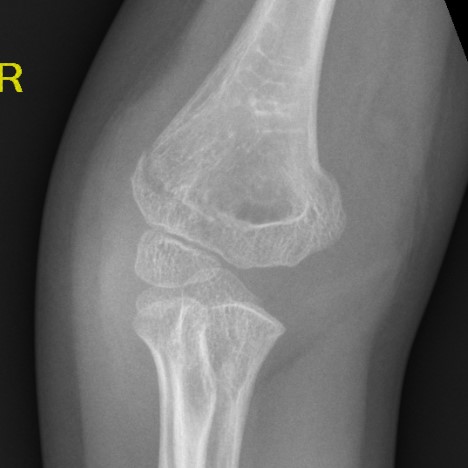
AVN Trochlear
Uncommon
Produces fishtail deformity
- deepening of trocheal groove
- DDx: trochlear AVN / central growth arrest / non reduced intercondylar fracture
- can be associated with early degenerative changes
- could consider epiphysiodesis of remaining growth plates, but usually well tolerated