Epidemiology
Second most common site of AVN
Much less common than hip OA
Usually presents late as shoulder non weight bearing
Typically not isolated - in multiple joints
Etiology
Most common non traumatic cause is corticosteroids
Similar causes as hip (AS IT GRIPS 3C)
Alcohol / Steroids / Idiopathic / Trauma
Gout, Gauchers
Rheumatoid / radiotherapy
Infection / increased lipids / inflammatory arteritis
Pancreatitis / pregnancy
SLE / sickle cell / smoking
Chronic renal failure / chemotherapy / Caisson's disease
Blood Supply
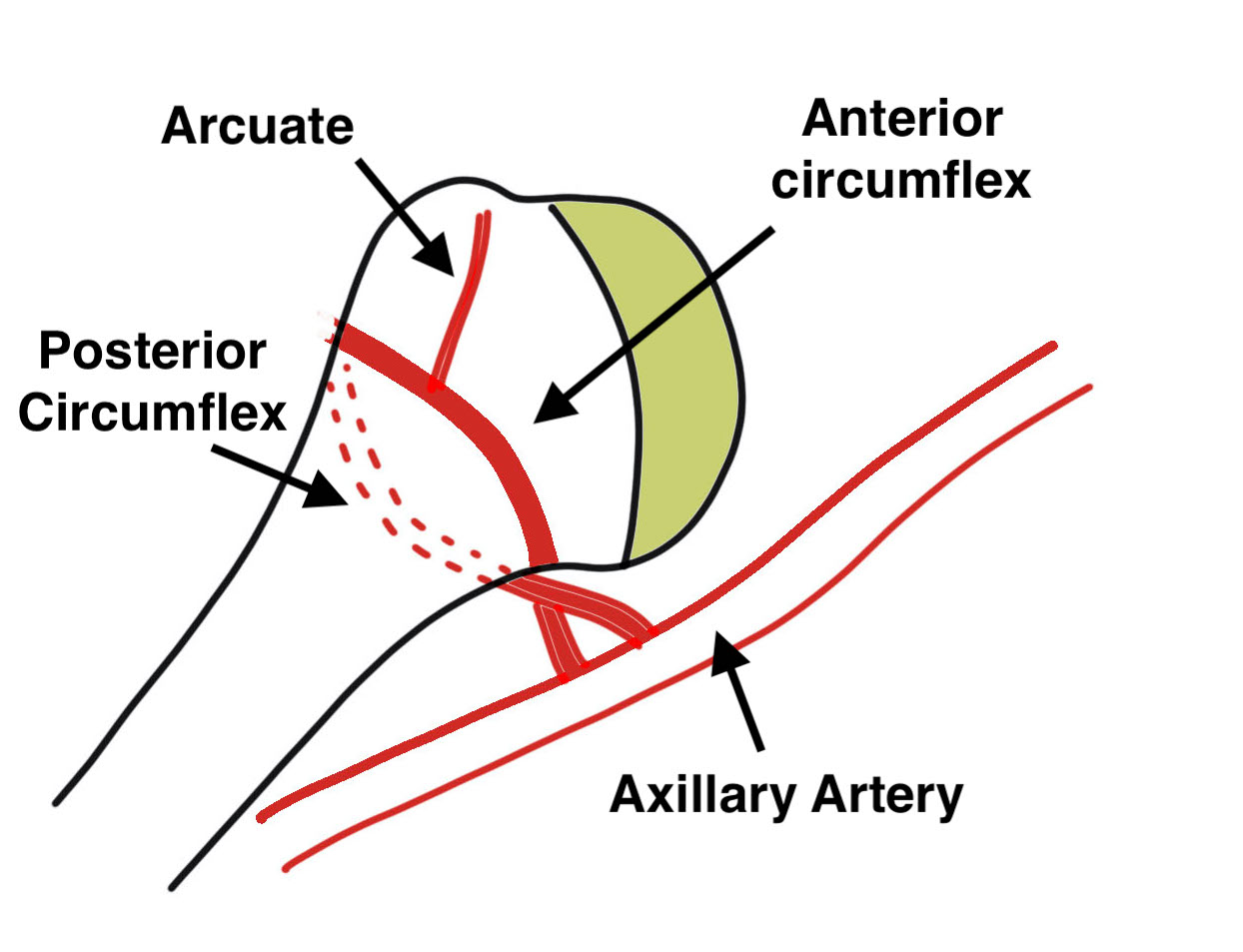
1. Anterior Circumflex Humeral Artery (36%)
- primary blood supply
- becomes arcuate artery
- runs lateral aspect bicipital groove
2. Posterior Circumflex Humeral Artery (64%)
- collateral circulation
- supplies head in setting of GT / LT fracture
3. Via rotator cuff
Natural History
Variable
- difficult to predict
- somewhat related to etiology
- sickle cell disease tend not to progress to arthroplasty
- steroid induced far more likely
Less severe than femoral
- non weight bearing
- less conforming joint
- scapulothoracic motion
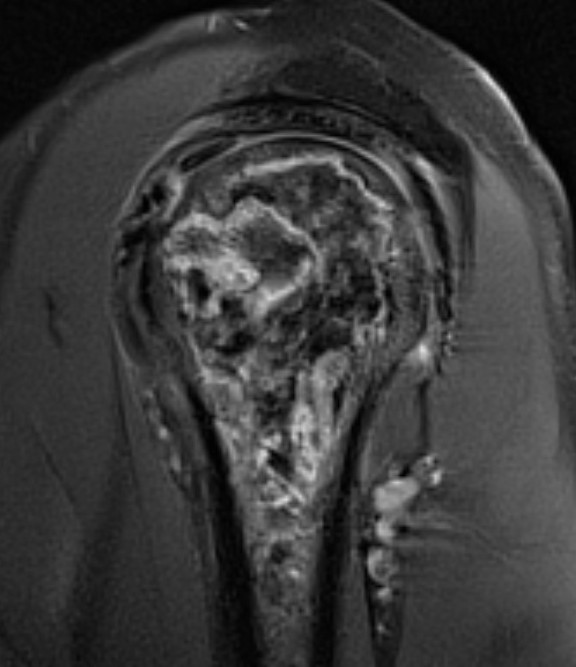
Pathology
Superior head collapse at 90° mark
- area of peak contact stress in abduction
- glenoid rarely affected
- soft tissue and subscapularis rarely contracted
Classification / Cruess modification of Ficat-Arlet
Stage I - pre-xray change / diagnosed on MRI
Stage II - sphericity maintained / sclerotic changes in superior central head / crescent sign


Stage III - mild flattening articular surface

Stage IV - significant humeral collapse with loss integrity joint surface


Stage V - degeneration extends to involve glenoid

Symptoms
Pain is major problem well before loss of range of motion
MRI


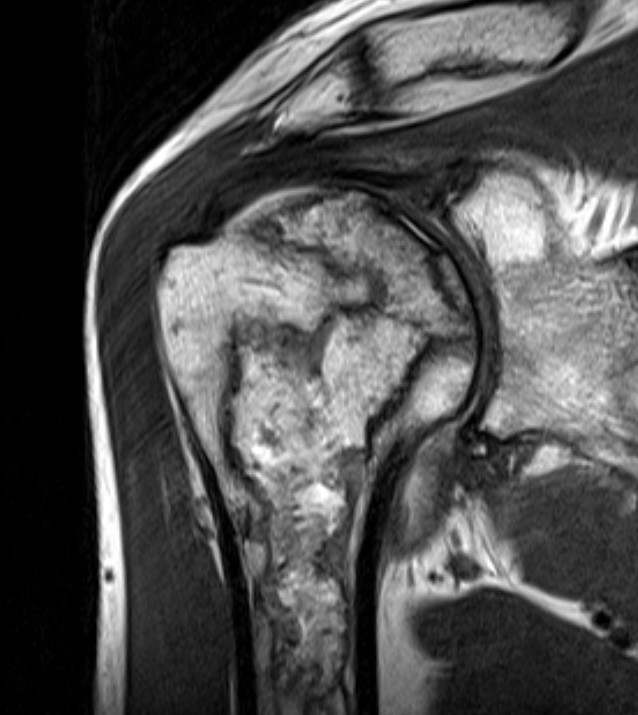
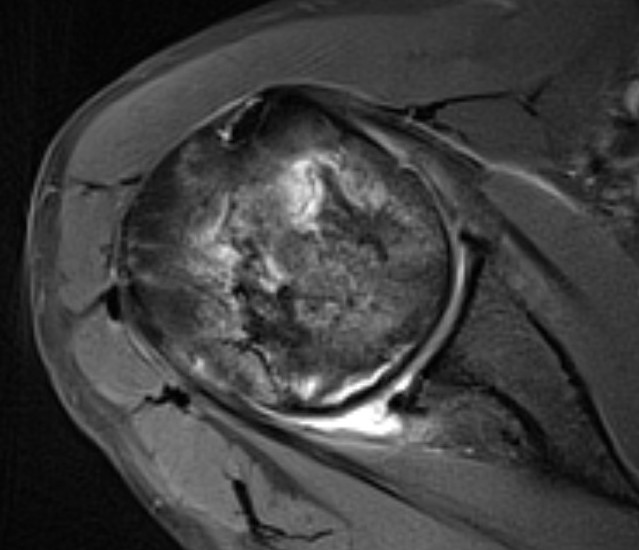
Sensitivity and specificity approach 100%
T1
- areas low signal intensity on T1 representing edema
- areas of high signal intensity thought to represent blood flow
T2
"Double line sign"
- highly specific for AVN
- inner bright line representing granulation tissue
- outer dark line representing sclerotic bone
Nonoperative management
Remove insult
Corticosteroids, alcohol
Maintain current shoulder ROM / Halt Progression
A. Physiotherapy
B. Limit overhead activities
- joint reaction force greatest > 90o
C. Bisphosphonates
Agarwala et al. J Orthop Surg Res 2019
- bisphosphonates for non femoral head AVN
- 20 patients, 5 with shoulder AVN
- combined oral and IV treatment
- 50% reduction in analgesia needs after 6 weeks
- MRI showed complete resolution in 17 / 20 (94%) at 1 year
Operative
Core Decompression
Concept
Decrease intra-osseous pressure & increase blood flow
Indications
Stage 1 / 2 - pre-collapse
Technique
Arthroscopy Technique Article decompression + fibular graft
Results
- core decompression in 63 shoulders all stages
- looked at improvement in UCLA scores
- 94% / 88% / 70%/ 14% success for stage I / II / III / IV
Alkhateeb et al. JSES Int 2021
- systematic review of core decompression in sickle cell
- one paper showed evidence of improved pain scores post procedure
- one paper demonstrated all cases went on to collapse
- may not prevent or delay progression of disease
Arthroplasty
Results
- 52 aTSA and 67 rTSA for shoulder AVN
- matched to controls in database
- similar improvements in ROM and PROM's to non AVN patients
Australian Joint Registry Shoulder Replacement for AVN 2021
- revision rate aTSR 11.4% at 5 years (compared with 7.2% for OA)
- revision rate rTSR 6.5% at 7 years (compared with 4.5% for OA)
- revision rate hemiarthroplasty 9.9% at 7 years (compared with 9.7% for OA)
