

Indications
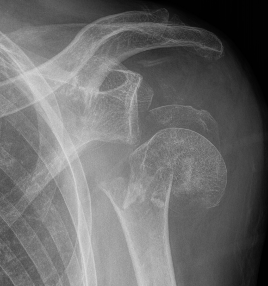
Rotator cuff arthropathy
Four part proximal humerus fracture
Revision shoulder arthroplasty
? Shoulder osteoarthritis with intact rotator cuff in older patients

Revision rate
Australian Joint Registry 2024
| Indication | 1 year | 5 year | 10 year | 14 years |
|---|---|---|---|---|
| Rotator cuff arthropathy (n=20,500) | 2.3 | 4.2 | 5.4 | 6.1 |
| Osteoarthritis (n=24,000) | 1.9 | 3.5 | 5.0 | 6.7 |
| Fracture (n=8,000) | 3.1 | 4.8 | 5.9 | 5.9 |
Design

Anatomic shoulder arthroplasty in cuff deficient shoulders
High failure rate
- superior migration / edge loading
- rocking horse phenomenon
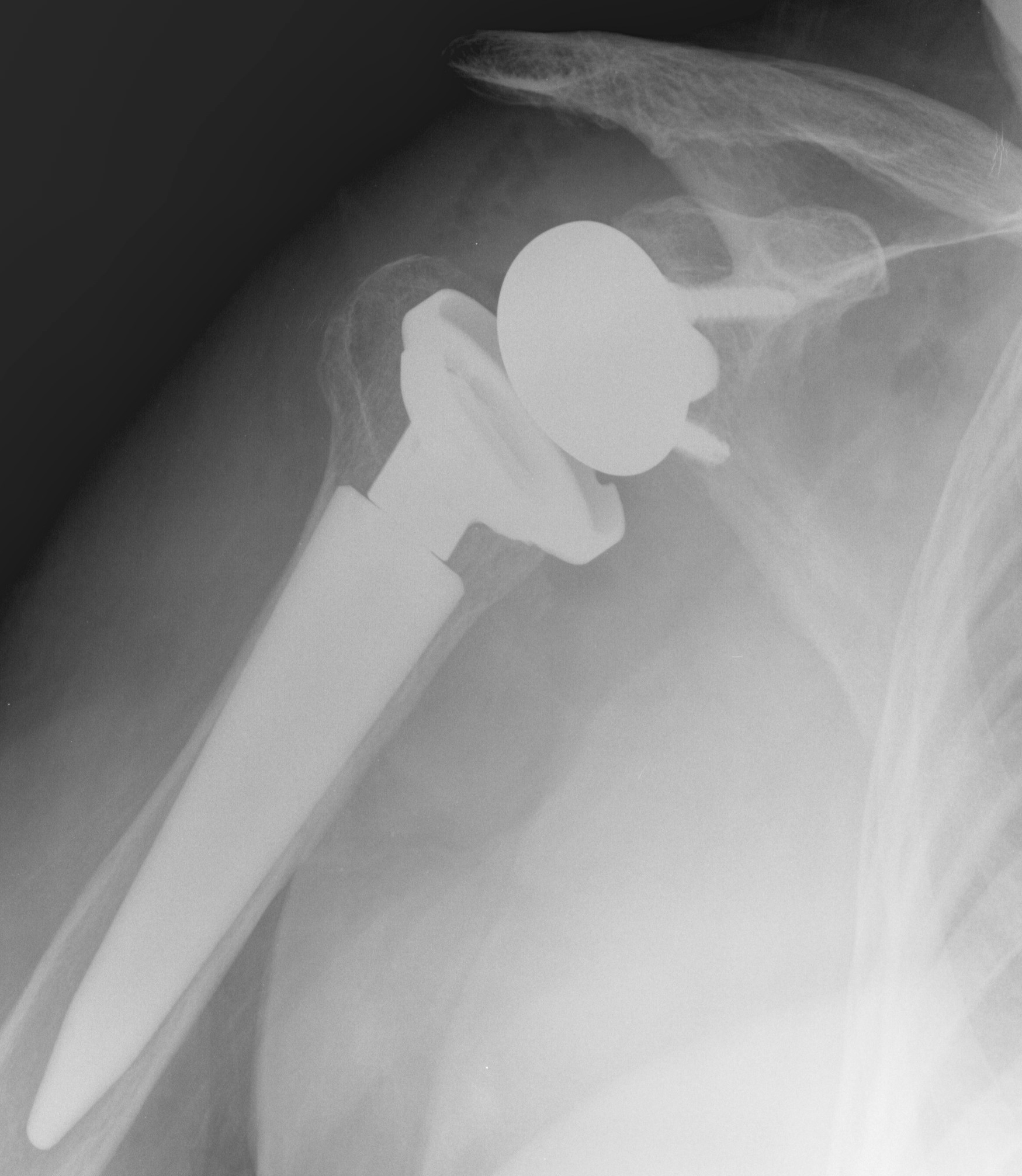
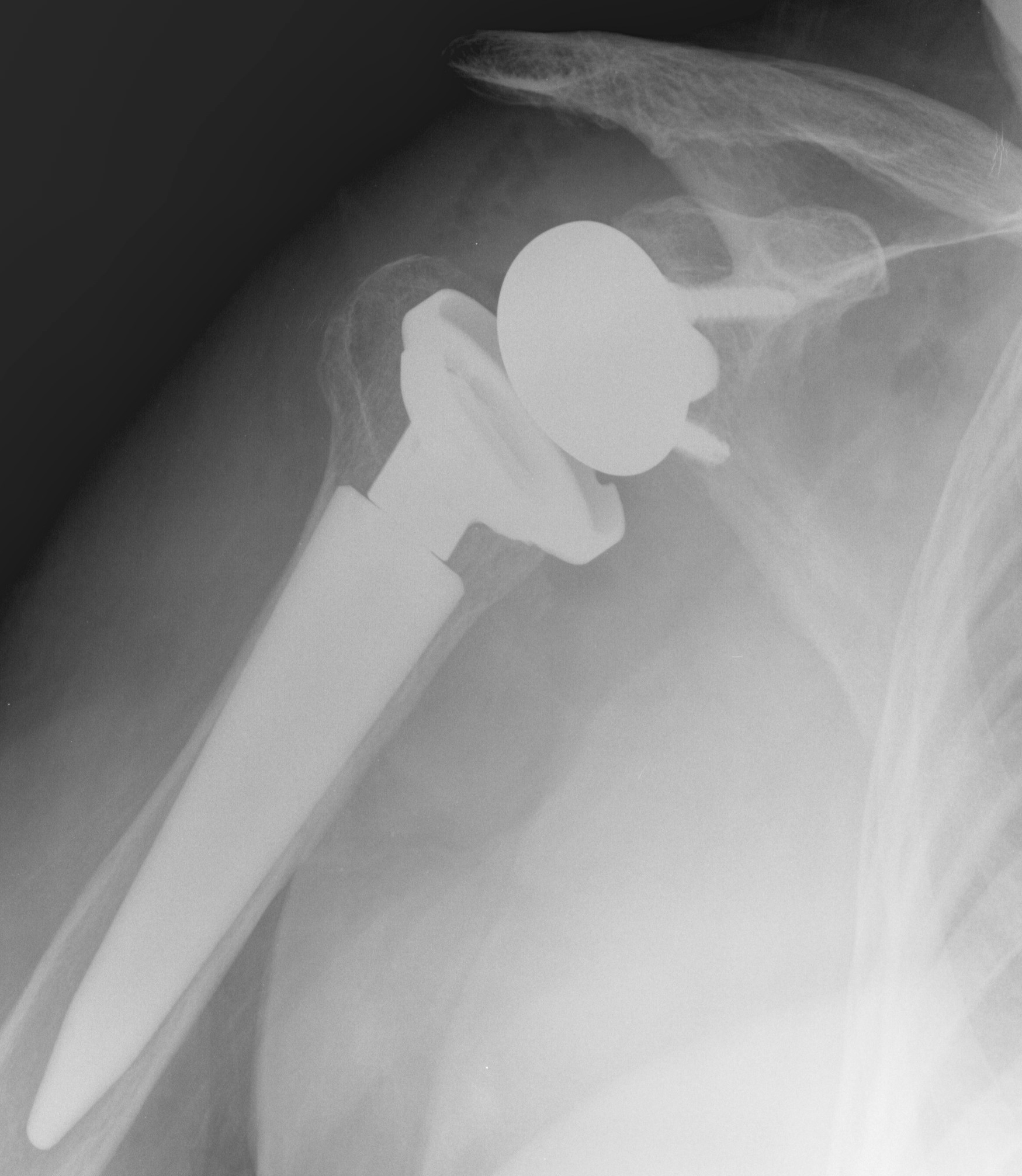
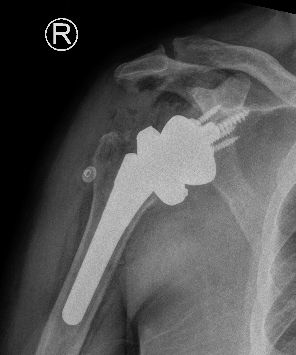
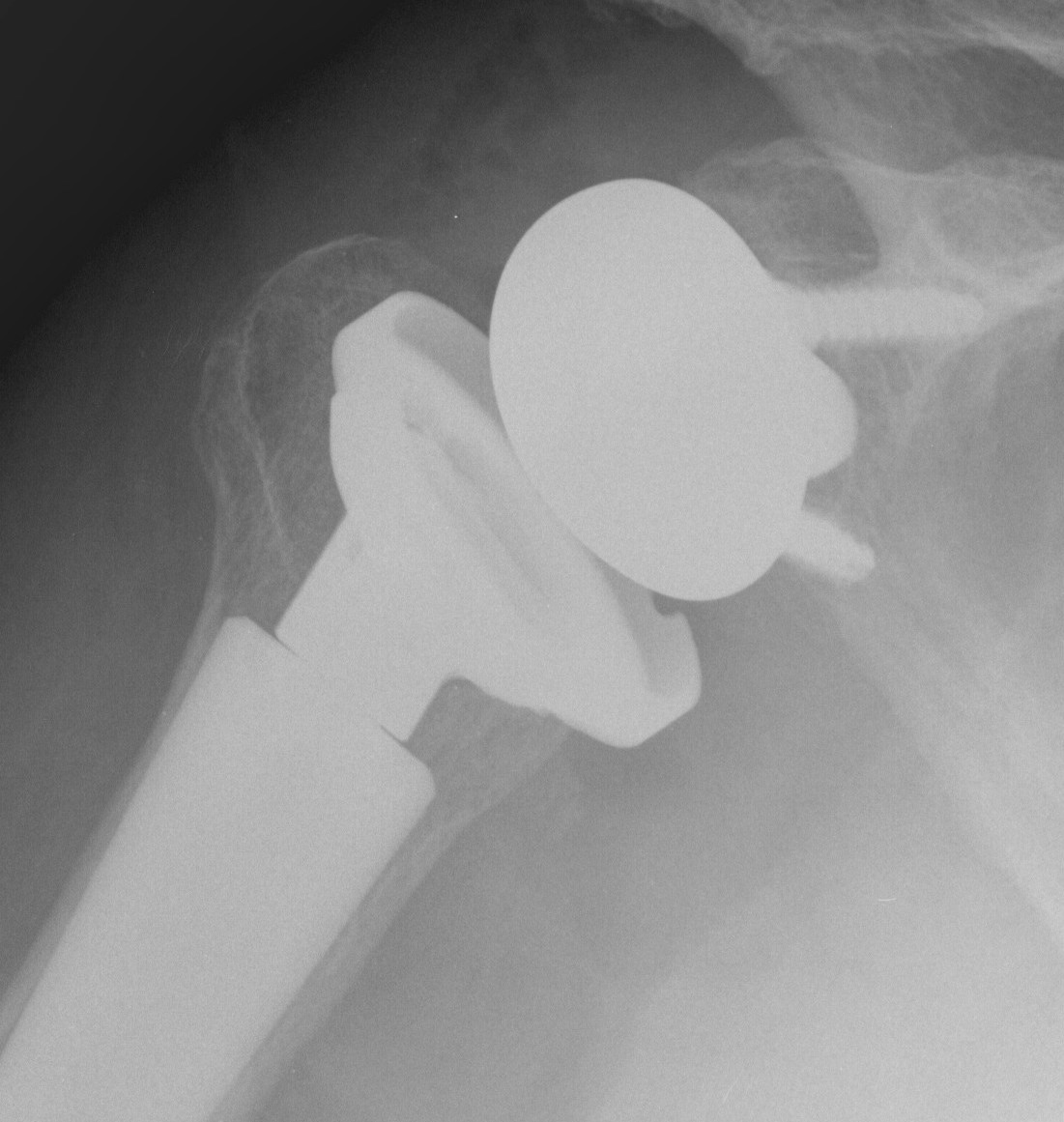
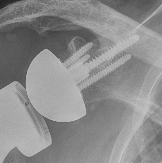
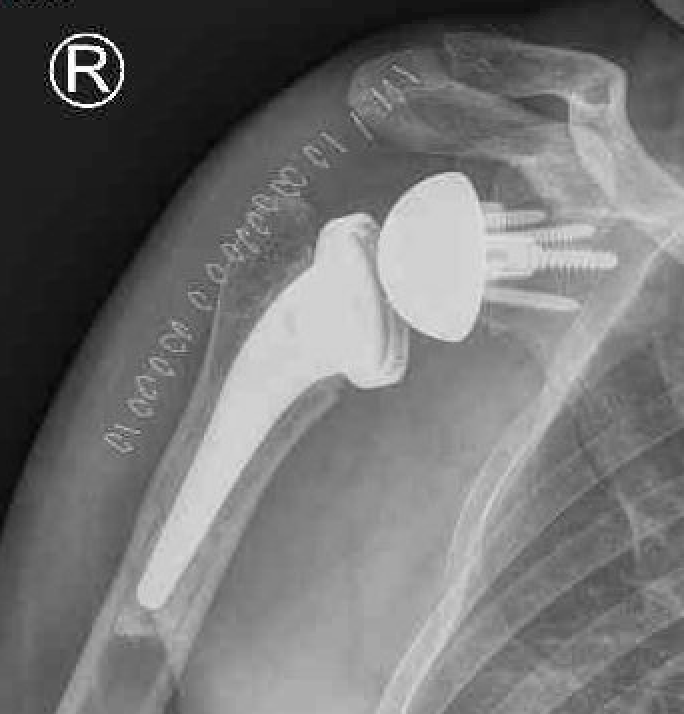
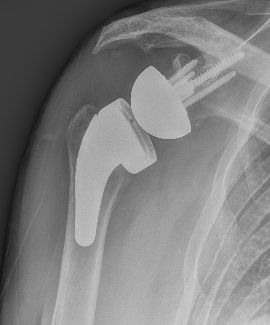
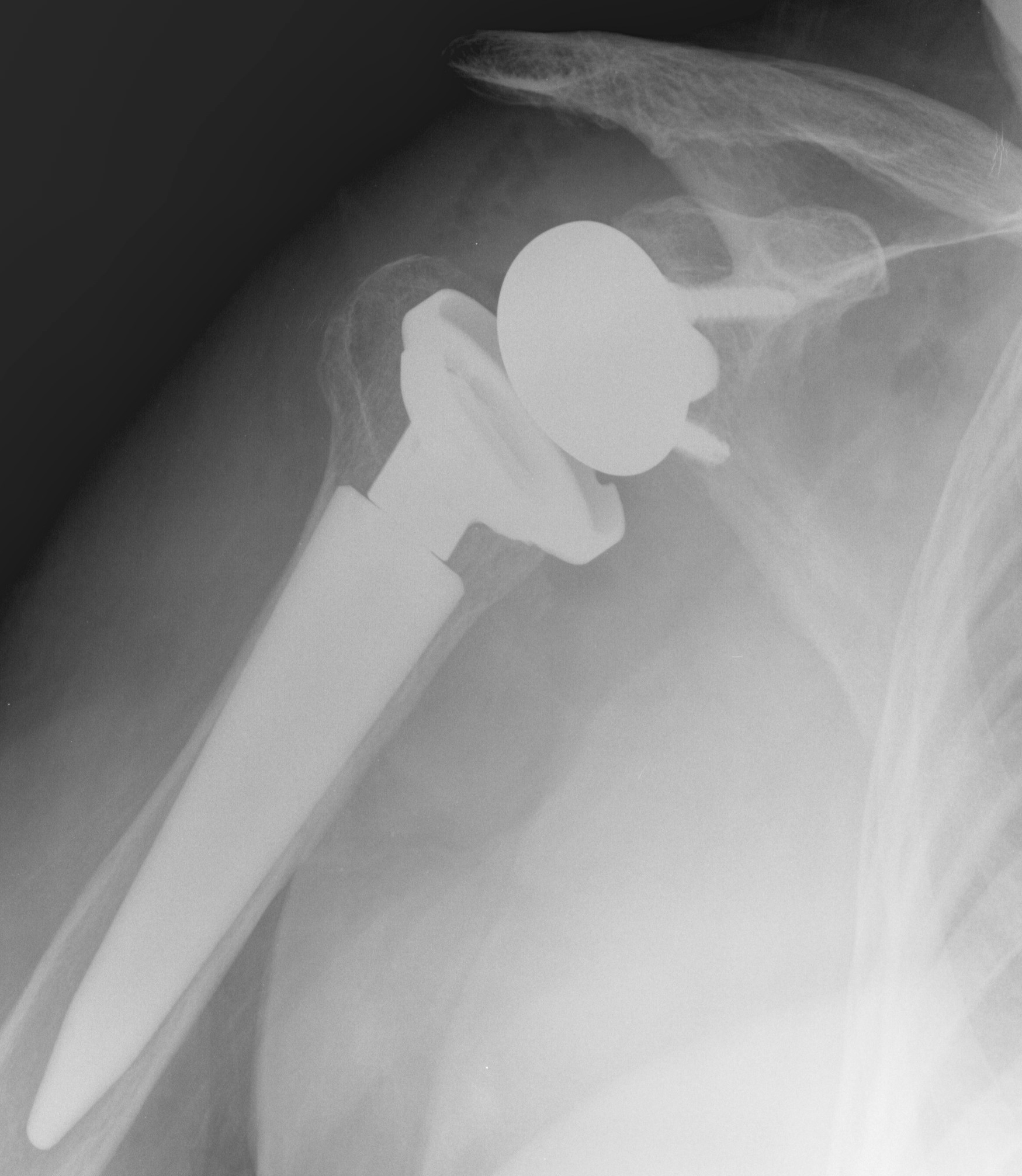
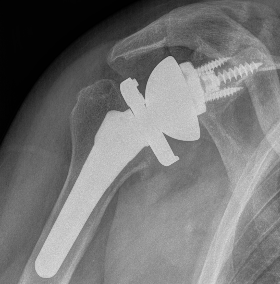
Reverse shoulder arthroplasty
Reverse
- socket in proximal humerus
- ball in glenoid
- center of rotation shifted medially and distally
- allows deltoid to apply compressive force and stabilize joint in absence of rotator cuff
Paul Grammont in 1985
- humeral component concave
- glenoid component / glenospere convex
- glenoid component uncemented with peripheral screws and central plug
- center of rotation shifted medially to glenosphere with humerus distal
Center of rotation


Increased lateralization of center of rotation
| Glenoid center of rotation | Humeral component | Four options |
|---|---|---|
|
Medialized or lateralized Based upon glenosphere thickness |
Medialized or lateralized Distance between the intramedullary canal axis / center of rotation of the humeral liner |
Medialized glenosphere / medialized humerus (MGMH) Medialized glenosphere / lateralized humerus (MGMH) Lateralized glenosphere / medialized humerus (MGMH) Lateralized glenosphere / lateralized humerus (MGMH) |
|
Humeral angle Inlay verus only Liner thickness |
- systematic review of rTSA
- medialized versus lateralized center of rotation
- better external rotation (20 v 8 degrees) and lower notching (7% v 48%) with lateralized COR
Bearing surfaces


Metal versus poly glenosphere. Lima SMR options
Australian Joint Registry 2024
| Bearing surfaces | 1 year | 5 year | 10 year | 14 year |
|---|---|---|---|---|
| Metal / XLPE (n=4,000) | 2.1 | 3.3 | 4.3 |
|
| Non XLPE / Metal (n=14,500) | 1.9 | 3.7 | 5.4 | 7.3 |
| XLPE / Metal (n=4,800) | 1.6 | 2.9 | 4.3 | 5.8 |
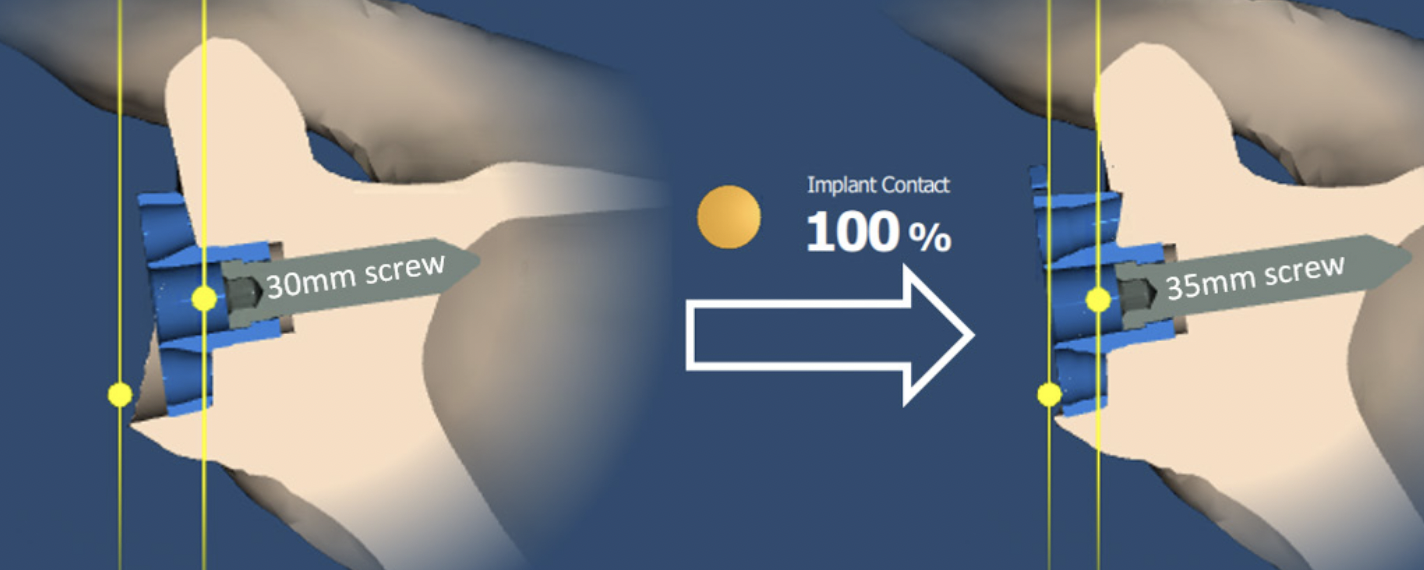
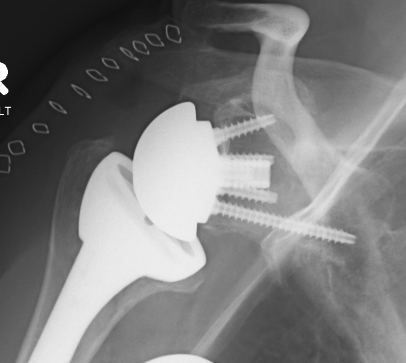
Glenoid component
Metaglene / baseplate
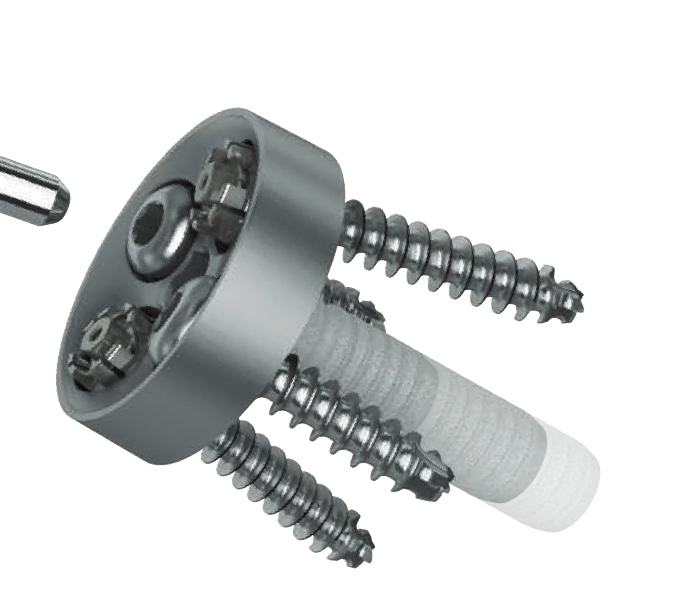
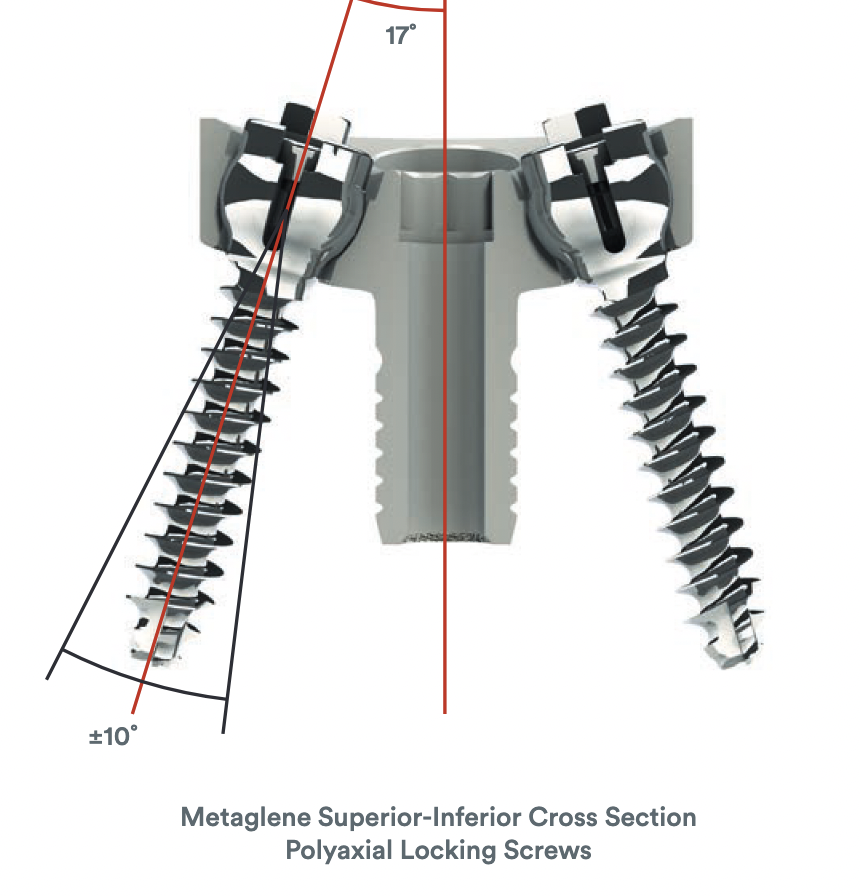
Depuy Synthes Delta Xtend
Design
- uncemented
- coated central peg
- secured by compression non locking screws + locking screw
- +/- variable angle to allow inferior screws along scapular spine / superior screw into coracoid
Glenoid augmentation
Indication
- usually for superior wear in rotator cuff arthropathy
- may be needed for posterior glenoid wear with rTSA for glenoid osteoarthritis
Zimmer Biomet Signature One Glenoid Augments
Wilcox et al Bone Joint J 2022
- systematic review of bone graft v glenoid augments for glenoid deficiency in rTSA
- higher complication rate with bone graft (9% v 3.5%)
- higher revision rate with bone graft (2% vs 0.6%)
- systematic review of bone graft v glenoid augments for glenoid deficiency in rTSA
- equal complication rates 11%
- similar revision rates (bone graft 4.5% vs augment 3.7%)
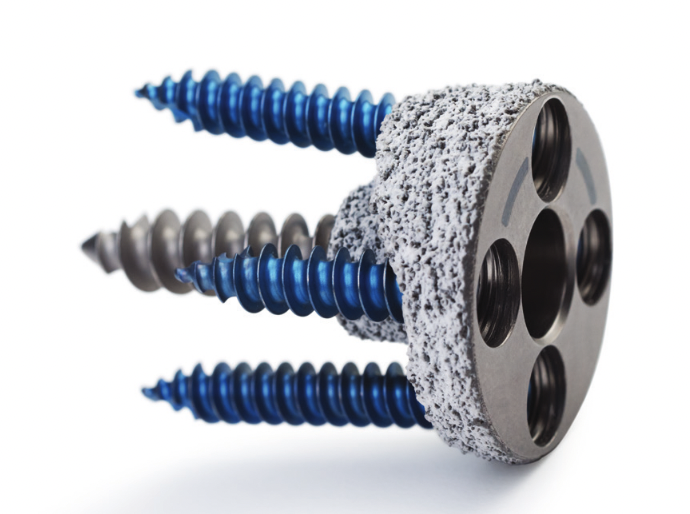
Glenosphere

Depuy Synthes Delta Xtend
Design
Press fit / morse taper onto baseplate
Lateralized / thicker options - limit scapular notching
Eccentric options - shift center of rotation inferior, limiting scapular notching
Size
Australian Joint Registry 2024
| Glenosphere size | 14 year |
|---|---|
| < 38 mm | 6.5 |
| 38 - 40 mm | 7.0 |
| > 40 mm | 6.4 |
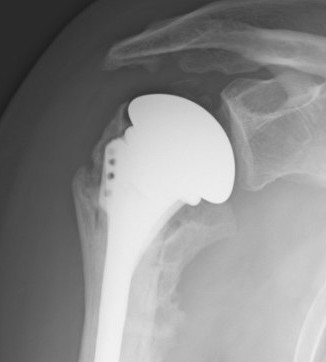
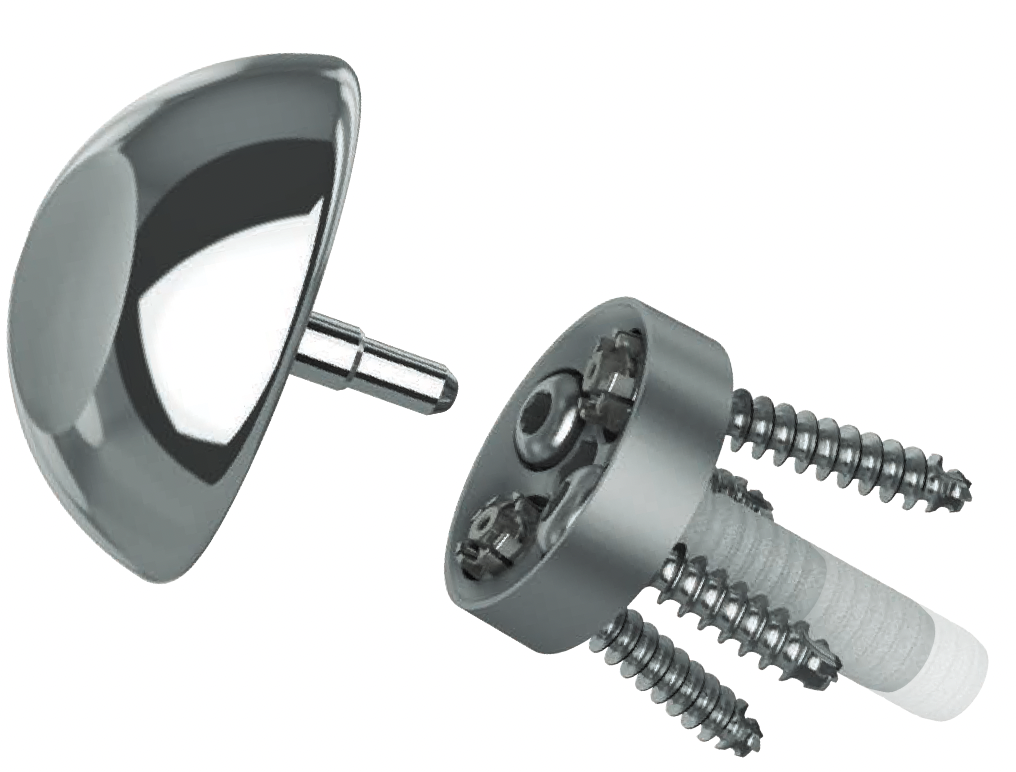
Humeral component
Retroversion
- systematic review of humeral version in rTSA
- 14 studies and 1200 patients
- < or > 20°
- at or > 20° of retroversion associated with better clinical outcomes and ROM
Fixation


Depuy Synthes Delta Xtend

Australian Joint Registry 2024
| Fixation | 1 year | 5 year | 10 year | 14 year |
|---|---|---|---|---|
| Uncemented (n=21,000) | 1.9 | 3.5 | 5.1 | 6.9 |
| Hybrid (humerus cemented) (n=2,600) | 1.9 | 3.1 | 4.5 | 4.9 |
Stem length
Australian Joint Registry 2024
| Stem length | 1 year | 5 year | 10 year | 14 year |
|---|---|---|---|---|
| Short <100mm (n=10,000) | 2.0 | 3.3 | 4.3 | 5.7 |
| Conventional > 100mm (n=13,500) | 1.8 | 3.6 | 5.4 | 7.3 |
Stemless
Kostretzis et al Musculoskeletal Surgery 2021
- systematic review of 13 studies and 500 patients
- 3.3% humeral associated complications
- 1.4% humeral component revision
Inlay versus onlay
Inlay - humeral tray sits within a prepared cavity in humerus
Onlay - humeral tray sits on the prepared cut surface of the humerus
- systematic review of inlay versus only humeral components
- no difference in clinical outcomes or ROM
- inlay - increased scapular notching
- onlay - increased scapular spine fractures
Outcomes
Clinical outcome
- systematic review of 1600 rTSA with minimum 5 year follow up
- 88% good or excellent patient reported outcomes
Range of motion
- systematic review of rTSA
- mean improvement of 56° in active flexion
- 50° in active abduction
- 14° in active external rotation
- systematic review of 1600 rTSA with minimum 5 year follow up
- active forward flexion 126° ± 13°
- active abduction 106° ± 11°
- active internal rotation 6° ± 2°
Rotator cuff arthropathy versus fracture
Paras et al J Shoulder Elbow Surg 2022
- systematic review of rTSA for RC arthropathy v 3 or 4 part fracture
- worse outcome scores and ROM for rTSA in fracture
Patients > 70 with GHJ OA and intact rotator cuff
Dragonas et al J Should Elbow Arthroplasty 2023
- systematic review of aTSA v rTSA in older patients with intact rotator cuff
- 1472 aTSA and 1259 rTSA with minimum follow up of 2 years
- better outcomes with aTSA
- increased revision rate with aTSA
Kim et al J Orthop Traumatol 2022
- meta-analysis of 6 studies comparing aTSA and rTSA with intact cuff
- no difference functional scores
- better external rotation with aTSA
- increased glenoid loosening with aTSA
- increased notching with rTSA
Survival
Australian Joint Registry 2024
| Indication | 1 year | 5 year | 10 year | 14 years |
|---|---|---|---|---|
| Rotator cuff arthropathy (n=20,500) | 2.3 | 4.2 | 5.4 | 6.1 |
| Osteoarthritis (n=24,000) | 1.9 | 3.5 | 5.0 | 6.7 |
| Fracture (n=8,000) | 3.1 | 4.8 | 5.9 | 5.9 |
| Age | 1 year | 5 year | 10 year | 14 years |
|---|---|---|---|---|
| < 55 (n=363) | 3.2 | 5.5 | ||
| 55 - 64 (n=2,500) | 3.5 | 6.0 | 9.3 | |
| 65 - 74 (n=9,500) | 1.8 | 3.6 | 5.4 | 7.2 |
| > 75 (n=11,500) | 1.6 | 2.7 | 3.8 | 4.3 |
| Gender | 1 year | 5 year | 10 year | 14 years |
|---|---|---|---|---|
| Male | 3.0 | 5.1 | 6.7 | 9.5 |
| Female | 1.2 | 2.4 | 4.0 | 5.0 |
