
Mechanism
Direct fall onto shoulder / FOOSH
Fall off bicycle / sports
Incidence
Fractures of the clavicle are common
- 70% male
- 5% of all fractures
- 80% involve the middle third
Anatomy
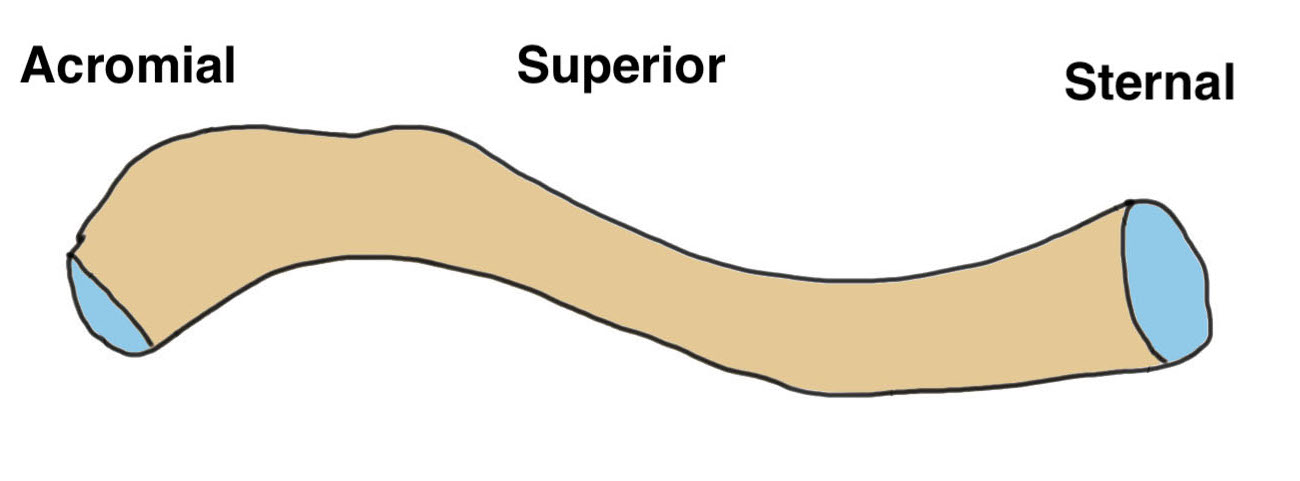
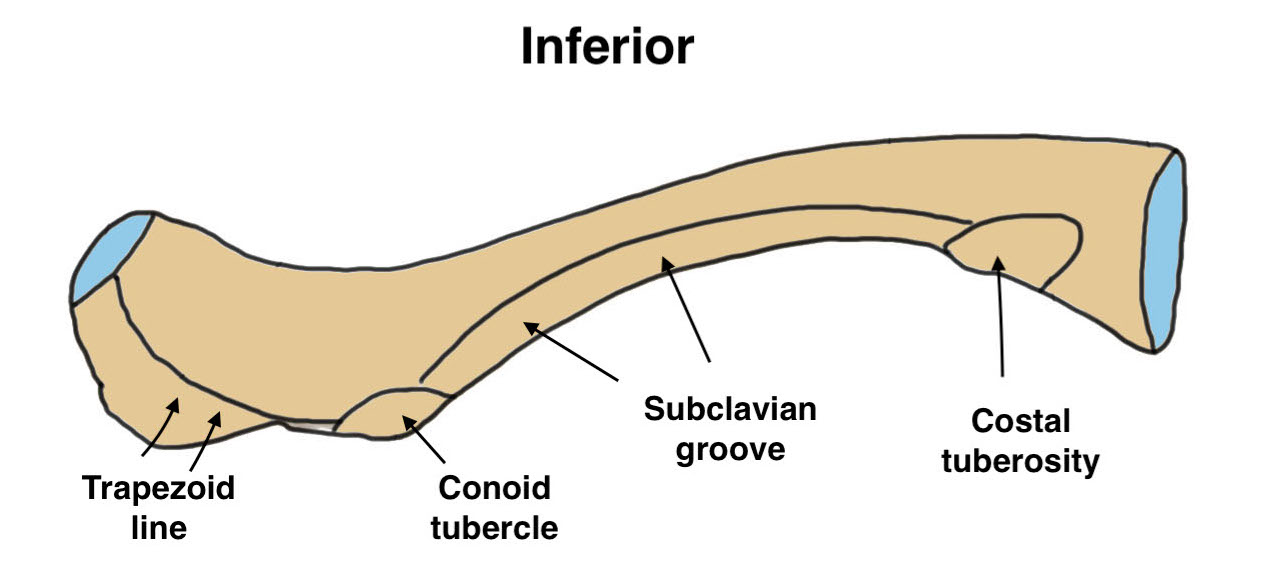
| Ossification | Shape | |
|---|---|---|
|
Intramembranus First bone to ossify / 5th week fetal life |
S shaped double curved bone Middle 1/3 is junction of 2 curves |
Rotates 40o with scapula is elevated |
| Most growth occurs at medial end | Medial convex anterior | Most rotation occurs with arm above shoulder height |
| Medial physis last to close at age 22 - 25 | Lateral convex posterior |
Classification clavicle fractures
Fractures may be divided into three regions of the clavicle
| Lateral | Midshaft | Medial |
|---|---|---|
|
Lateral 1/5 of clavicle Line drawn up from base of coracoid |
Intermediate 3/5 |
Medial 1/5 of clavicle Line drawn up from center first rib |
|
20% of clavicle fractures
|
70 - 80% | Rare |
 |
 |
Examination
Skin
- skin tenting / threatened skin
- compound wounds
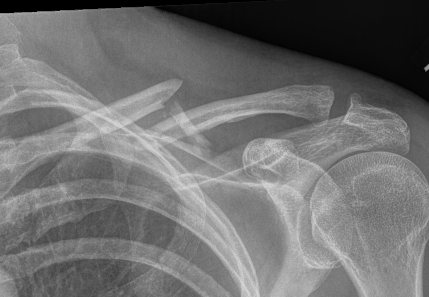
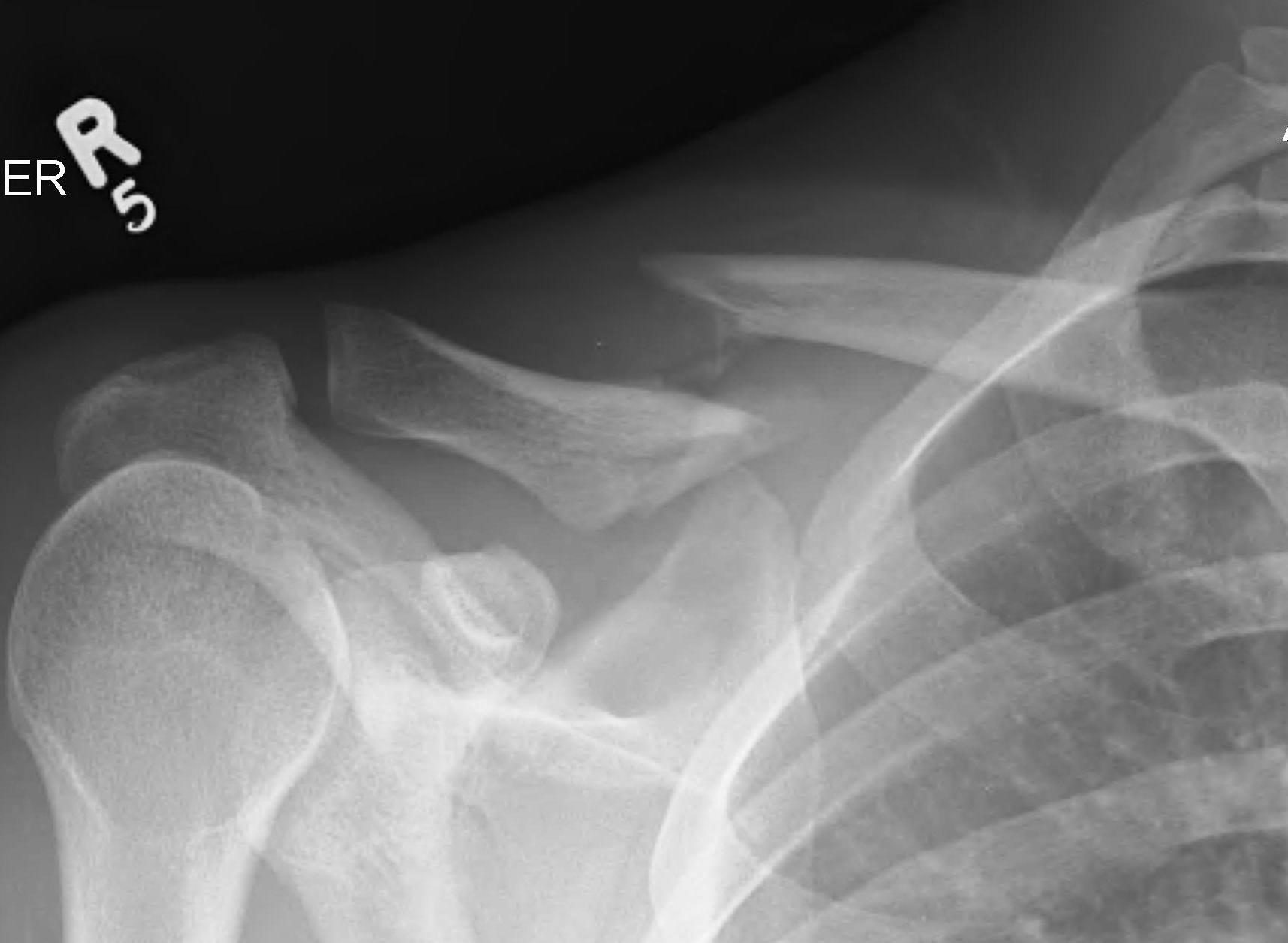
Xray
Shortening


Displacement
- the proximal fragment elevated by sternocleidomastoid
- lateral fragment sags down with weight of shoulder

Management
Operative indications
| Absolute | Relative |
|---|---|
| Compound fracture | Shortened / displaced |
| Skin tenting / skin under threat | Multitrauma |
| Floating shoulder |

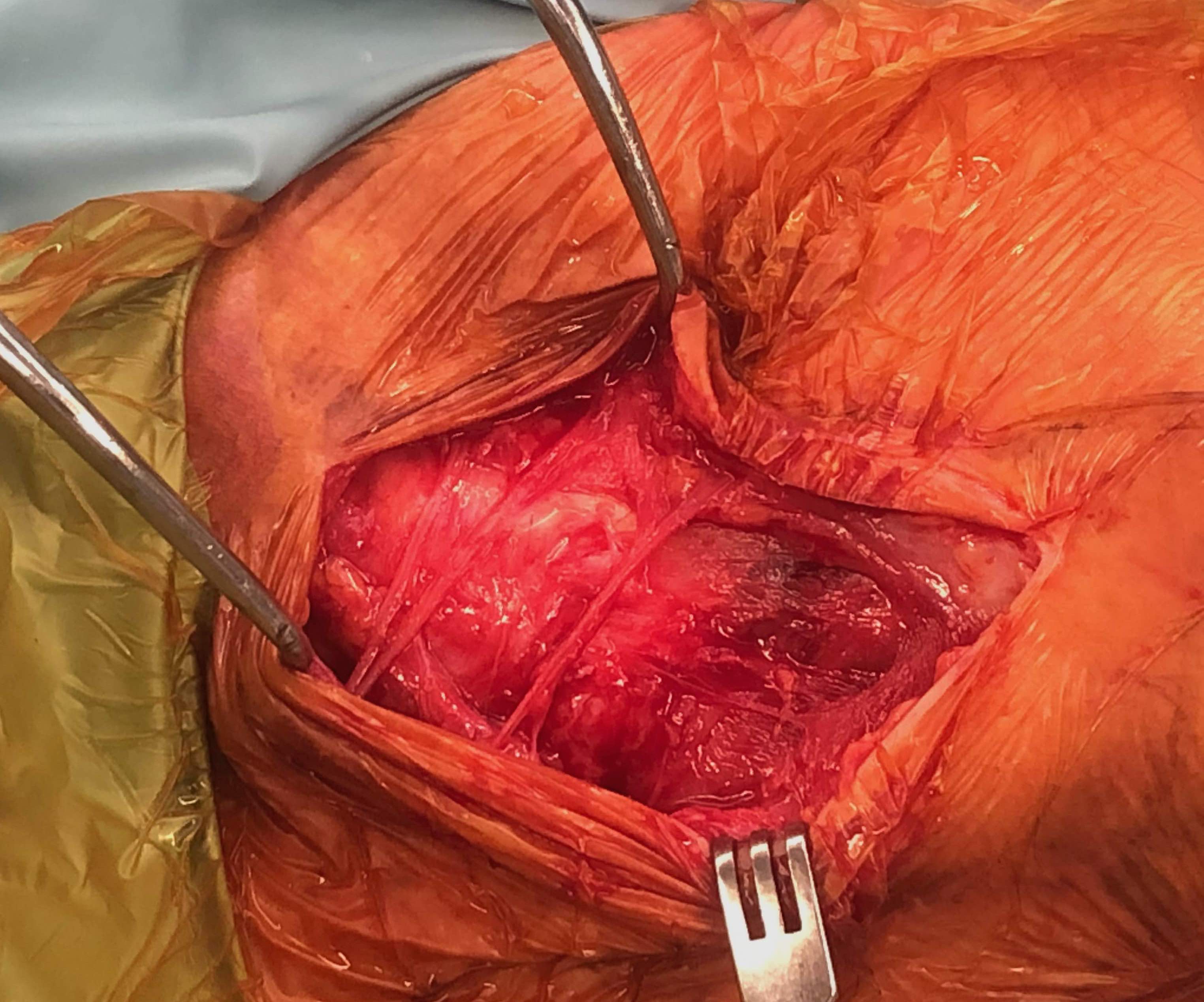
Compound clavicle fracture
Shorted / displaced midshaft clavicle fractures

Z shaped midshaft clavicle fracture
Operative versus Nonoperative management

Canadian Orthopedic Trauma Society JBJS Am 2007
- RCT of 62 operative v 49 nonoperative treatment of displaced midshaft clavicle fractures
- operative v nonoperative
- time to union: 16 v 28 weeks
- nonunion: 5% v 14%
- symptomatic malunion: 0 v 18%
- RCT of 200 patients with displaced clavicle fractures
- operative versus nonoperative
- nonunion: 1% v 15%
- no difference in outcome if union achieved
- RCT of 160 patients with displaced clavicle fractures
- operative versus nonoperative
- nonunion: 2% v 23%
- no difference in outcome if union achieved
Summary
Plate fixation of shorted displaced midshaft clavicle fractures reduces nonunion rates
Operative Management
Options
Plate fixation
Intramedullary screw
Plate fixation


Superior versus anteroinferior plates
Nourian et al J Orthop Trauma 2017
- systematic review of superior v anteroinferior plates
- no difference in outcome or union rates
- higher incidence sympomatic hardware with superior plates
Dual plating

- comparison of superior / inferior / dual plating with minifrag plates
- lowest rate of reoperation with minifrag plates
- reduced nonunion and reduced need to remove prominent hardware
Technique
Vumedi clavicle ORIF with plate video
Lazy beach chair
- square drape / free drape
- LA with Adrenalin
Transverse incision in Langer’s line
- ? identify and protect supraclavicular nerves
- divide platysmus as a layer to repair later
- clean and reduce fracture
- application contoured locking plate
- need 6 cortices each side
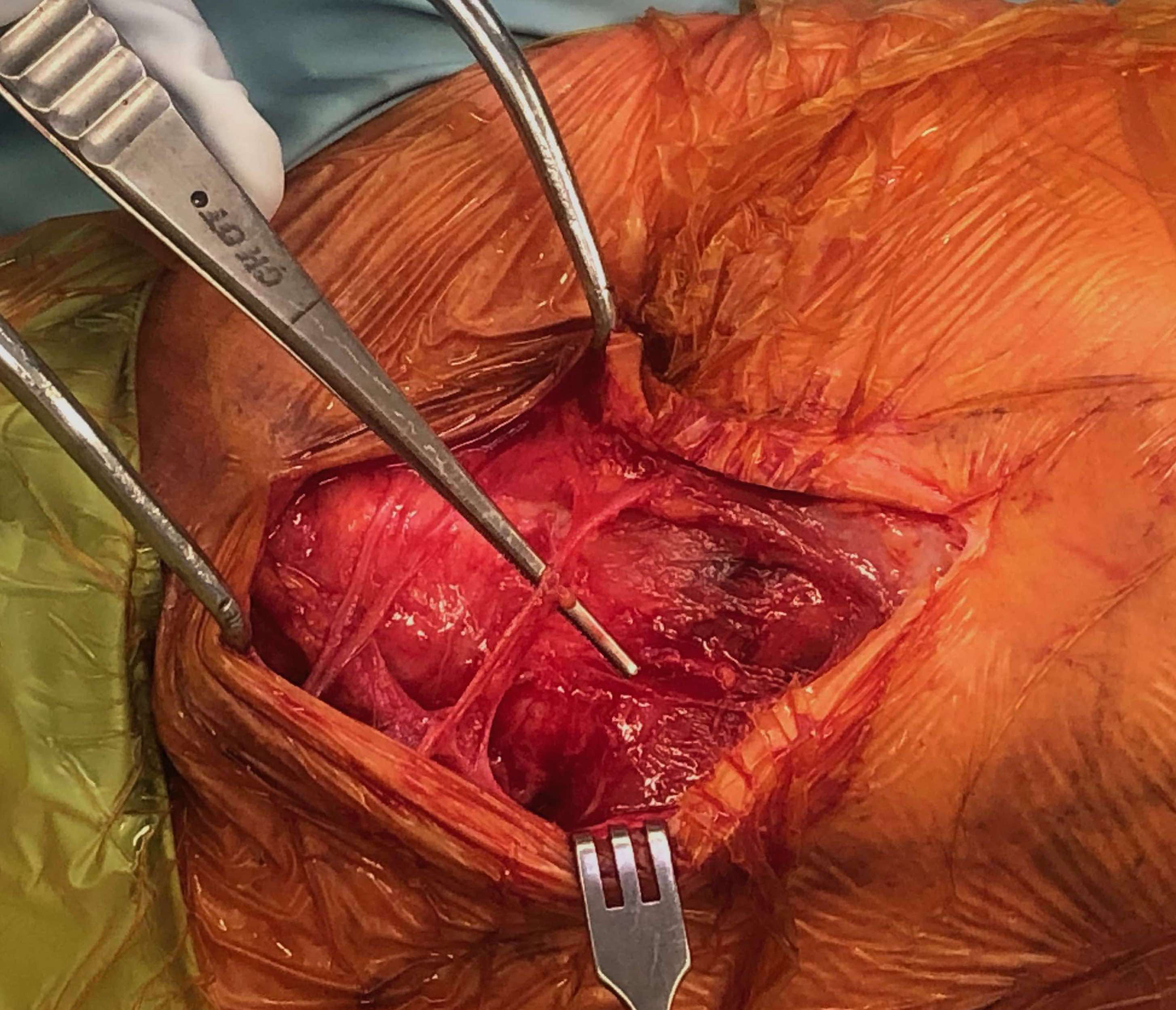
Supraclavicular nerve branches
Intramedullary screw

Indication
Displaced clavicle fractures
Minimal comminution
Results
- systematic review of plate versus IM screw fixation
- no difference in union rates / outcomes
- increased hardware removal with screw fixation
- increased refracture rate after plate removal
Fuglesang et al Bone Joint J 2017
- RCT of plate versus IM screw in 123 patients
- shorter duration of surgery with IM screw
- faster functional recovery with plate fixation
- slower function recovery with IM screw fixation in setting of increasing comminution
Technique
Vumedi surgical technique clavicle IM screw
Mini open approach to fracture
- drill medial fragment for screw
- pass cannulated wire through lateral fragment and out through skin
- reduce fracture and pass wire into medial fragment
- drill lateral fragment
- insert cannulated 6.5 mm screw
- needs to be between 80 and 110 mm
- check x-ray to ensure good medial fixation
Complications of operative management
Pneumothorax
Vascular injury
Brachial plexus injury
Infection / wound breakdown
Numbness
Painful hardware
Nonunion
Vascular injury
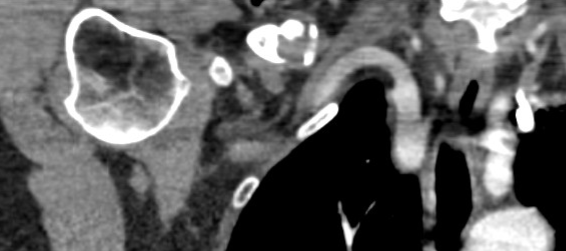
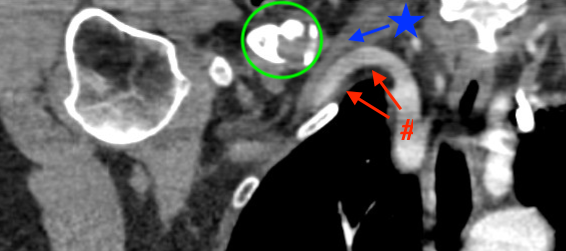
CT scan: green circle - clavicle nonunion, red arrows - subclavian artery, blue arrow - subclavian vein
Subclavian vein injury
Subclavian vein may be adhered to periosteum medially
- instrumentation medially and inferiorly must be subperiosteal
- careful with medial screws
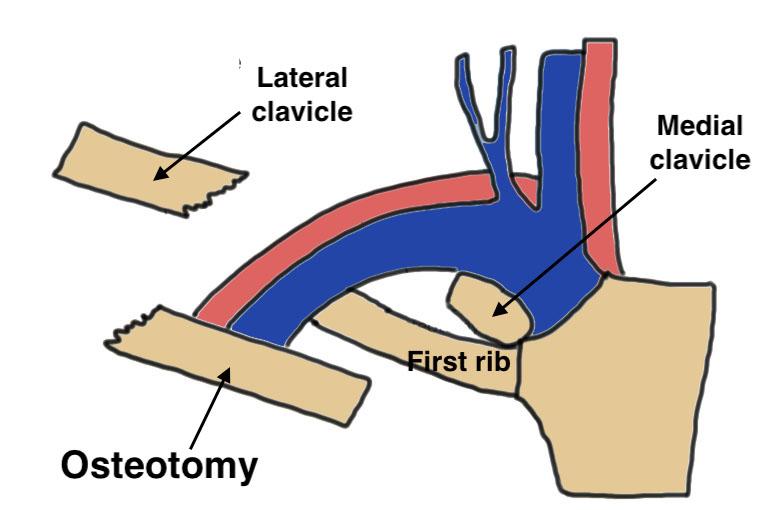
- may need clavicular osteotomy to control bleeding
- wet packs and head down to prevent air embolus
Clavicular osteotomy for subclavian vein injury PDF
Air embolus
Air enters from subclavian vein injury
- due to negative pressure
- enters right ventricle and causes and air lock
- poor saturation / high CO2
Patient must be put in immediate head down position
- prevent further air embolus with pressure / saline packs
- aspirate air from right ventricle
- vascular repair of subclavian vein
Subclavian artery pseudoaneurysm
Often delayed presentation
- intermittent claudication
- pulsatile mass
- treat with stent / bypass
Brachial plexus injury
Present postoperatively with
- severe radicular pain
- incomplete sensory / motor impairment
Jeyaseelan et al Bone Joint J 2013
- 21 cases of brachial plexus injury following clavicle plating
- usually C5/6, upper trunk
- all cases involved delayed fixation / average 19 days
- brachial plexus tethered by scar to clavicle
- recommend extensive scar release in delayed fixation
Infection / wound breakdown

Periprosthetic fracture

Nonunion




Technique
Vumedi dual plating clavicle nonunion
Results
Muhlenfeld et al J Clin Med 2024
- 44 patients with nonunion
- union rate with plate: 94%
- union rate with plate + bone graft: 96%
Malunion



Symptoms
Pain, weakness, fatigue, parasthesia
Theory
Clavicle shortening causes altered scapular mechanics
- scapular winging
- increased thoracic outlet symptoms
- disrupted ACJ and SCJ
Technique
Vumedi surgical technique video clavicle malunion
Results
- 15 patients with clavicle malunion
- average shortening 2.9 cm
- osteotomy + plate
- 1 non union
- 8/12 patients with weakness and pain improved
