Xray Assessment
A: Alignment
B: Bony
C: Canal
D: Disc
S: Soft tissues
Goals of surgery
1. Correct deformity
2. Restore stability
3. Decompress neural elements if required
MRI
Advantage
- defines level of conus
- may need anterior rather than posterior surgery if lesion above conus
Denis's 3 column Classification 1982
> 3 columns injured with translation
- unstable
Posterior column
- supraspinous / infraspinous ligament / ligamentum flavum
- neural arch (lamina / pedicle / facet joints / spinous process)
Middle column
- PLL, posterior disc & annulus
- posterior half vertebral body
- most important
Anterior column
- ALL, anterior disc & annulus
- anterior half vertebral body
Denis Classification
1. Compression fracture
- anterior column only

2. Burst fracture
- anterior and middle column disrupted
- widening of pedicles on AP
- decreased posterior body height compared to anterior
- may have retropulsed fragment
- this occurs at top of vertebral body between pedicles
- obscured by pedicles on lateral xray

3. Flexion-distraction
- distraction of posterior structures
- disruption of middle column
- splaying of spinous processes on AP and lateral
- bony or ligamentous
- chance injury (pure bony)
- anterior column intact / no translation
4. Fracture-dislocation
- all three columns disrupted
- characterised by translation
Surgical Indications
1. Neurology
- decompress
- complete v incomplete
2. Deformity
- correct deformity
Gertzbein SRS 1992
- 1109 patients
- kyphosis >30° associated with increased back pain
3. Stability
- prevent neurology
- prevent deformity / late pain
4. Multi-trauma patient
TLISS (Thoracolumbar Injury Severity Score)
Spine Trauma Study Group
- 3 issues
- calculate a score
- gives an indication if patient needs surgery
1. Injury Mechanism
Compression 1
Burst 2
Rotation 3
Distraction 4
2. Posterior Ligament Complex
Intact 0
Suspected 2
Definite 3
3. Neurology
Nil 0
Nerve root 1
Complete cord 2
Incomplete cord 3
Cauda equina 3
10 is maximum score
- < 4 no treatment
- 5 or more - surgery
- 4 - either way
Burst fracture
- 2 points for burst
- 2 for indeterminate posterior injury
- usually no neurology
- 4 in total
Timing
Incomplete neurology
- emergency
- especially if neurology worsening
- have more time if neurology stable
- i.e. time to get MRI
Complete neurology
- not an emergency
- surgery still indicated
- gain 1 or 2 neurological levels (crucial in C spine)
- prevent syrinx
- prevent development of neuropathic pain
- aid nursing / rehabilitation
Bohlman 1985 JBJS
184 thoracic spine fractures with complete cord injury
- no recovery with or without OT
- posterior fusion only to speed recovery
17 incomplete cord injuries treated with laminectomy
- 7 became worse
- hence contra-indicated
8 incomplete cord injuries treated with anterior decompress+ fusion
- all improved
- decreased rehabilication time by 50% in operative group
Approach
Posterior
Indications
- flexion distraction
- fracture dislocation
- compression fractures
- +/- burst
Requires integrity of posterior column
- Gaines score
Issue
- disruption of posterior column
- higher risk of dural tears
Anterior
Indication
- decompression required
- i.e. burst with retropulsed fragment
- perform corpectomy via anterior approach
Anterior & Posterior
Gaines / Load sharing Classification
Enables decision be made
- short segment posterior stabilisation v
- anterior decompression and stabilisation
Gaines Class >/=7 = failure with pedicle screw construct alone
A. Comminution vertebral body on lateral X-ray
1. <30%
2. 30-60%
3. >60%
B. Apposition of Fragments
1. Minimal displacement
2. 2 mm or <50% of body
3. > 2 mm or >50% body
C. Deformity Correction
1. Kyphosis 3o or less
2. 4-9o
3. >10o needed
Score of 3-9
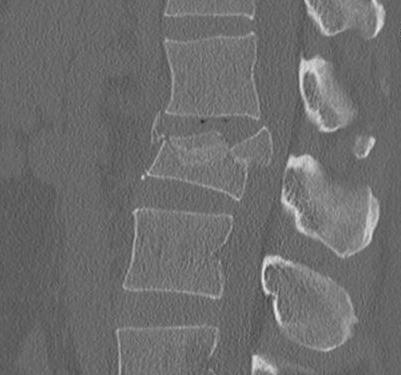
1. Compression Fractures
DDx
- burst
- pathological
CT scan
- xray only 25% accurate distinguishing compression from burst
- indicated if anterior body height < half posterior body height
- i.e. > 50% anterior wedging
- assess integrity of middle column / look for retropulsed fragments
Operative Indications
- kyphosis > 30o
Non Operative Management
- elderly - mobilise
- young - extension orthosis / TLSO
- check standing X-ray 2/52
- ensure kyphosis < 20 - 30o
Surgery
- posterior approach
- instrumentation
2. Burst Fracture
Characteristics
- axial load
- most common thoracolumbar junction
- retropulsed fragment here causes conus
Definition
- anterior & middle column disrupted
- posterior column injured but no displacement / translation
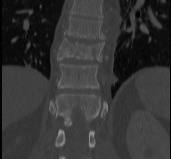
X-ray
- pedicle widening on AP
- posterior body height decreased on lateral < 50%


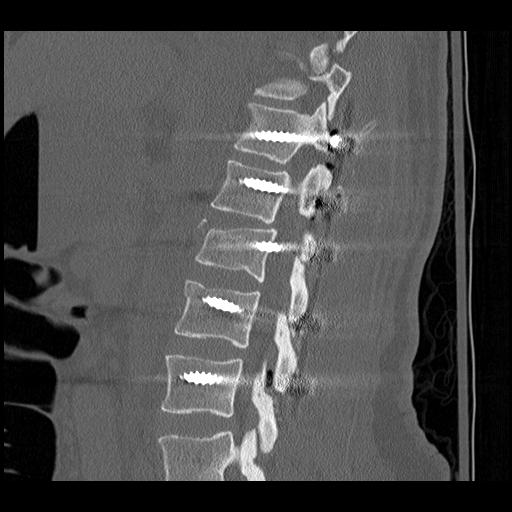
CT
Look for canal compromise
- cord signal change
- kyphotic deformity

Retropulsed fragments
- always between pedicles
- typically one or two main fragments (saloon door)
- assess canal compromise



MRI
- HNP
- cord signal change
- assess posterior ligament integrity
- assess level of conus medullaris


Clinically
1. High association abdominal trauma
- duodenum, aorta, spleen
2. Neurology
- complete v incomplete
- from retropulsed fragments
Non-Operative management
Indications
- no neurology
- no deformity / < 30o kyphosis
- stable
TLSO
Surgical Indications
TLISS > 4
- usually means neurology
Kyphotic deformity
Failure non operative
Anterior corpectomy and strut graft
Indication
- decompression of retropulsed fragments in patient with neurology

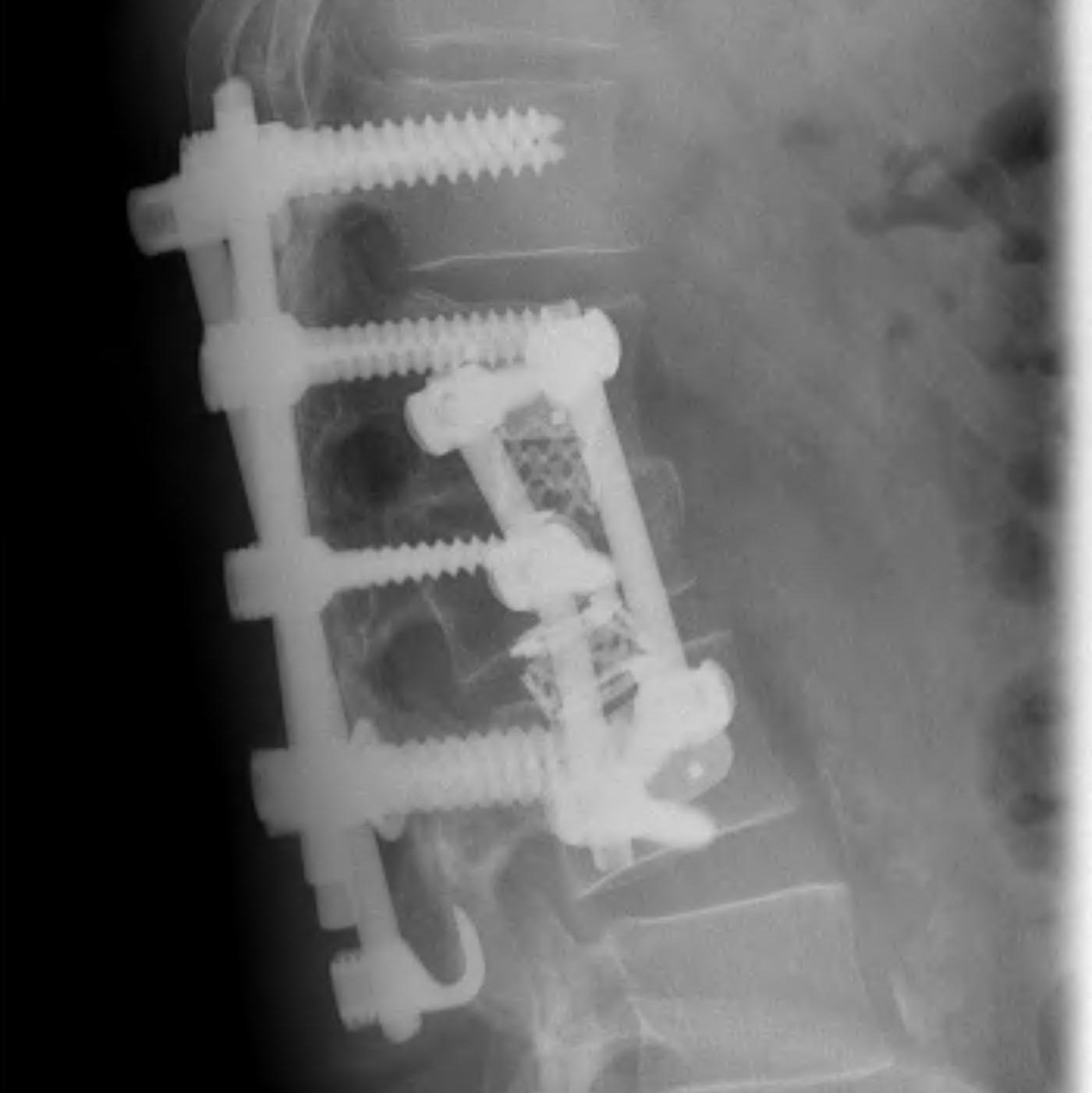

Technique
- approach as per level
- thoracoabdominal for T11 - L1
- thoracotomy for T2 - T10
- remove disc above and below and remove vertebral body
- remove fragments / need to know if 1 or 2
- screws in vertebral body above and below
- 2 screws in a lateral plane
- insert fibular strut allograft / titanium cage
- augment with cage
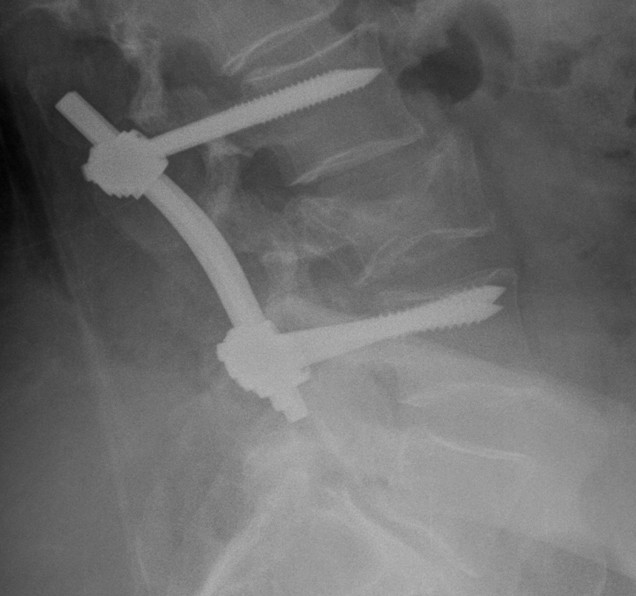
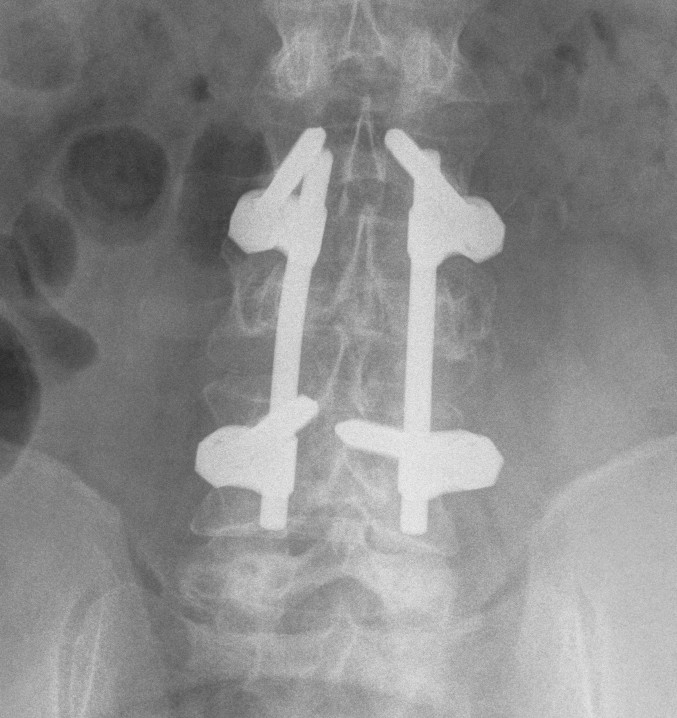
Posterior instrumentation
Indication
- < 7 gaines criteria
- no neurology
Technique
- ligamentotaxis clears canal / PLL acts as bowstring
- pedicle screws lumbar, avoided in thoracic
- use transverse process and pedicle hooks in thoracic
- bone graft inserted via pedicles
- need to do before 5 days post injury


3. Flexion Distraction
Definition
Seat belt injuries
- injury all 3 columns
- posterior fails in tension
- anterior and middle in distraction
- anterior undisplaced with no translation
Associated injuries
1. Hollow viscus
Anderson et al J Orthop Trauma 1991
- 2/3 have injury to hollow viscus
- duodenum very common as second part fixed
- 1/4 have hemoperitoneum from mesenteric laceration
2. Ileus
- very common
- manage NBM / NGT
Types
1. Pure bony
- through vertebral body
- Chance fracture
2. Ligamentous
- through disc space and facet joints


3. Combined
- rare injury
Management
Bony chance
- can heal in hyperextension orthosis
- assess reduction in brace / < 15o kyphosis
- otherwise can fix with pedicle screws and TP hooks of same vertebrae
Ligamentous
- treat surgically as unstable and ligament heals poorly
- respond well to short segment posterior instrumentation
- above and below disc space injured
- i.e. T12 and L1 instrumented



Neurology / deformity
- reduction and posterior stabilisation
- add decompression if required
4. Translational - Fracture / Dislocation



Background
3 Column injury
- high energy
- unstable by definition
- required operative stabilisation
- profound neurological deficit common
Types
1. Shear
2. Flexion-distraction with translation
3. Flexion-rotation
- unilateral facet dislocation
- < 25% translated
Management
Incomplete or no neurology
- rare
- great care must be taken to not worsen patient
- MRI to exclude disc / determine level of conus
Options
- posterior approach / decompression / reduction / stabilisation
- consider anterior approach if HNP / above level conus