Definition
Forward slip of one vertebra relative to inferior one
Classification
Wiltse "DID TIP"
Dysplastic
Isthmic
Degenerate
Traumatic
Iatrogenic
Pathological
1. Dysplastic 20 %
Congenital Dysplasia of Upper Sacrum
- occurs at L5-S1
- hypoplasia of superior facets of S1
- dysplastic L5/S1 facet joints
Usually around 6 years old
Spina bifida ccculta common
- more unstable
Prone to more severe slips
Most high grade slips are dysplastic
2. Isthmic 50 %
Pars Discontinuity / Defect
- L5 /S1 80%
- unilateral or bilateral
- can have a pars defect at L4/5
- typically adolescent
- due to repetitive stress with fracture
- increased in competitive sports eg gymnastics, football
- is a genetic predisposition due to increased pelvic incidence
- tend to be mild and non progressive
Tend to present in 2 groups
- some present in young patient
- some present in adulthood when the disc degenerates and foramina compressed


3 types
A Stress fracture
B Elongated type

C Acute fracture
3. Degenerative
2° to Facet OA
- L4/L5
- > 40 years old
- associated with DM
- F>M
- compared with lytic the disc tends to be preserved

4. Traumatic
Bilateral acute fracture through neural arch outside pars
- i.e. hangman's fracture
5. Iatrogenic
Post surgical
6. Pathological
Pathological weakening of neural arch or pedicle
- OI / Larsen / Marfan's / tumour
Epidemiology
Occurs after walking
- never present at birth
Spondylolysis seen in 5% causcasion population
- 15% develop spondylolithesis
Gender
- more common in boys
- girls more severe slips
NHx Lytic
Early NHx
- by early adulthood L5-S1 disc narrowed
- anterior sacrum develops sclerotic lip
- further slip unlikely in adulthood
- will only progress whilst skeletally immature
Late NHx
- increased incidence of L5-S1 disc degeneration
- significant increase in LBP > 50% slip
- may develop nerve root pain when foramina compressed due to disc degeneration
Aetiology Isthmic
Fracture of pars
Lumbar extension concentrates shear stresses on thin pars
- inferior articular process of cranial vertebrae continuously impacts on pars
- nutcracker mechanism
Most common
- soldiers /weight lifters / footballer's
- female gymnasts 10%
FHx
- positive FHx in 15%
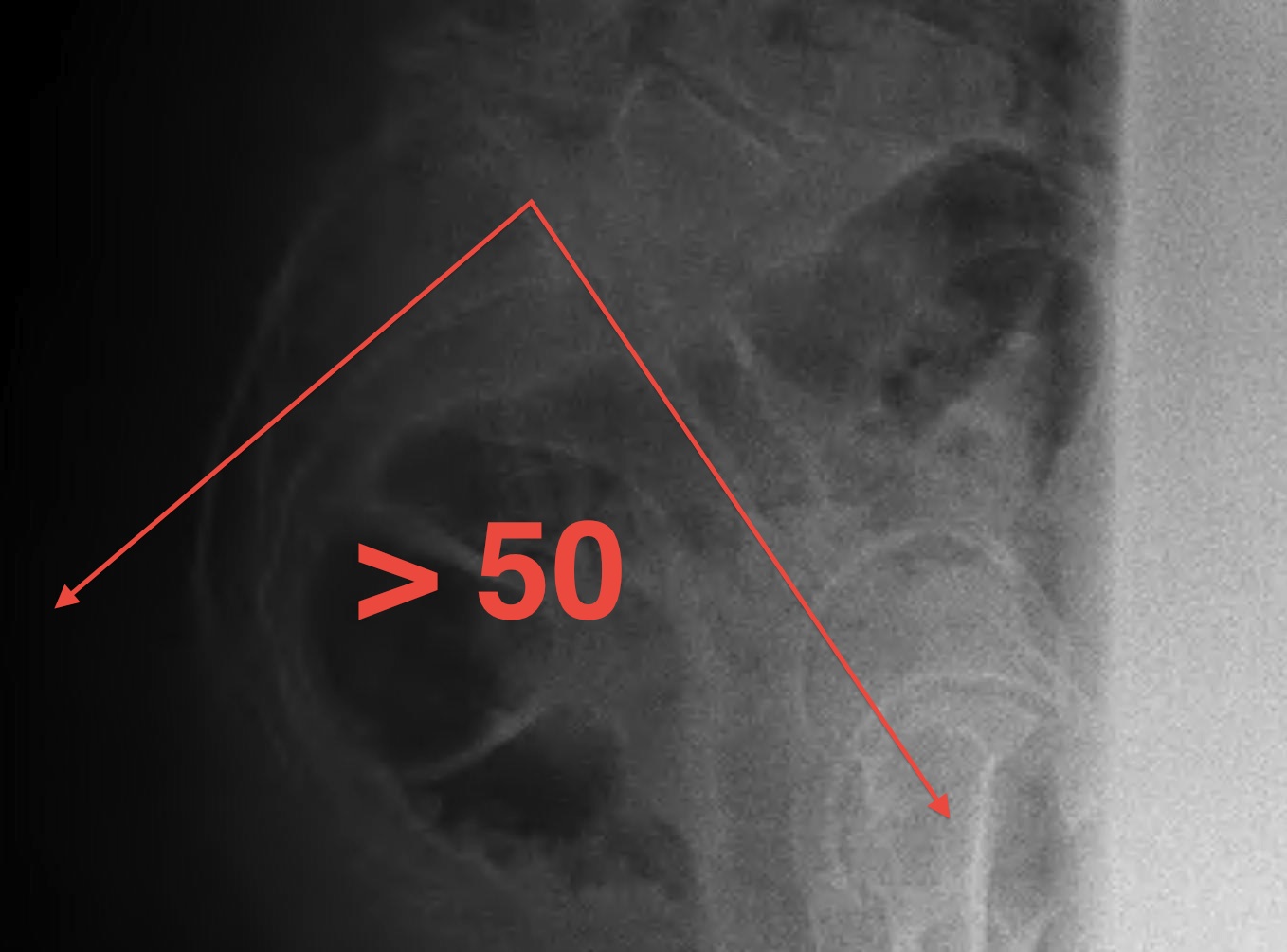
Pelvic Incidence
Isthmic associated with increased pelvic incidence > 50o
- patients have increase lumbar lordosis with increased shear stress
- predisposed to pars fracture if engage in certain sports with hyperextension
Measurement
- line superior border sacrum / sacral slope
- drop perpendicular line from centre of sacral slope line
- line to centre femoral head
- pelvic incidence is line between the two

Aetiology Dysplastic
Secondary to posterior element abnormality
- increased incidence of sacral spina bifida
FHx
- positive FHx in 33%
Pathology
1. Isthmic
Usually lower grades
- posterior elements left behind
- canal diameter increased
L5 nerve root compression
- fibrocartilage mass at pars defect
- stretched over posterior sacrum
2. Dysplastic
Higher grades
- severe lumbosacral kyphosis
- canal diameter decreased
L5 nerve root + cauda equina pressure
- intact neural arch of L5 pulled forward
Symptoms
Usually asymptomatic in children
- only 10% are painful
- pain usually in growth spurt adolescents
Back pain
- low back / buttocks & thighs
- initiated by strenuous activity
- repetitive flexion extension
- relieved by rest
Can often recall a specific inciting event
Neurology
- radicular pain
- exiting nerve root / usually L5 in both dysplastic and isthmic
Signs
Lumbar hyperlordosis
Lumbosacral step off with severe slips
Numbness in L5 area
Scoliosis
- increased incidence in symptomatic slip
- 25-50%
- more common with dysplastic
Spondylo-crisis
- acute presentation with severe back pain
- hands on knees, hips and knees flexed
- bladder and bowel dysfunction
Standing AP and Lateral X-ray
Findings
May miss subtle listhesis on supine XR
- spondylosis
- Meyerding classification
- slip angle
- sacral inclination
Spondylolysis

Definition
- radiolucent defect of pars
Types
- acute - narrow gap & irregular edges
- pars elongated & thinned
- chronic - wide gap with smooth sclerotic edges
Scotty Dog / Oblique Xray
- Ear (superior articular facet) / Nose (TP) / Eye (pedicle)
- Front leg (inferior articular facet) / Body (lamina and body with superimposed SP)
- Tail (superior articular facet of other side) / Back leg (inferior articular facet of other side)
- Neck (Pars and if Collar then has defect)


Meyerding Classification
Degree of slip compared with width of S1
- Grade I 0-25%
- Grade II 25-50%
- Grade III 50-75%
- Grade IV 75-100%
- Grade V > 100% / Spondyloptosis
Stability
- stable / slip < 50%
- unstable / slip > 50%

Slip Angle / kyphotic angle
Measurement
- line along inferior border L5
- line along superior border S1
Normally L5/S1 disc is in 20-30° lordosis
- angle is negative
As L5 slips forward it slips into kyphosis
- angle becomes positive
- sacrum becomes more vertical with high grade slips
- this worsens the kyphosis further
Dangers
- typically > 10° with dysplastic
- > 30° high risk progression progression
Sacral inclination
Angle between posterior border of sacrum and vertical
- > 60o associated with progression
Chronic Changes
Seen in older presentation
- anterior sacral erosion
- domed sacrum
- L5 Trapezoidal
- L5/S1 disc degeneration
Bone Scan
1. Diagnosis
SPECT
2. Prognosis
Hot lesion
- will heal
Cold lesion
- not healing
CT scan
Technique
- reverse gantry
Indication
- perform instead of obliques
- oblique x-rays have high radiation dose with little extra information compared with CT


MRI
Indication
- neurological signs
- rule out other diagnosis
DDx
Infection - vertebral OM / discitis
Tumour - osteoid osteoma / cord tumour
Herniated disc
Inflammatory - Scheuermann's / Ankylosing Spondylitis
Management
High Risks Progression
1. Clinical
- skeletally immature
- female
2. X-ray
- dysplastic slip
- grade III or IV (> 50%)
- slip angle / kyphosis > 30° (normal is -20° i.e. lordosis)
Non Operative
Indication
Minimal symptoms
Low risk progression
- isthmic
- mild slip (Meyerding I / II, slip angle < 30o)
Protocol
Observation until mature
- review annually to ensure no progression of slip
Consists of
- activity modification
- cease aggravating symptoms
- NSAIDS
- hamstring stretches
- brace
Brace
Indication
- spondylosis / grade 1 spondylolithesis
- acute / hot on bone scan
Theory
- attempt to heal pars fracture
- healing is not required for symptoms to settle
Type
- anti-lordotic
- 3/12 full time, no sport
- 3/12 full time with sport
Results
Debnath et al Spine 2007
- 42 patients with unilateral spondylysis hot on SPECT
- 6/12 non operative treatment including bracing
- 81% avoided surgery / complete resolution of symptoms
- remainder had CT confirmed non union and underwent unilateral pars fixation
Operative Management
Indications
1. High risk slip
- slip degree > 50%
- slip angle > 30o
- dysplastic
- skeletally immature
2. Progression of slip
3. Neurological symptoms
- L5 Radiculopathy / Stenotic symptoms / cauda equina
4. Debilitating pain
- spondylysis
- spondylolithesis
Options
1. Pars fusion
- painful spondylysis
- minimal spondylolithesis
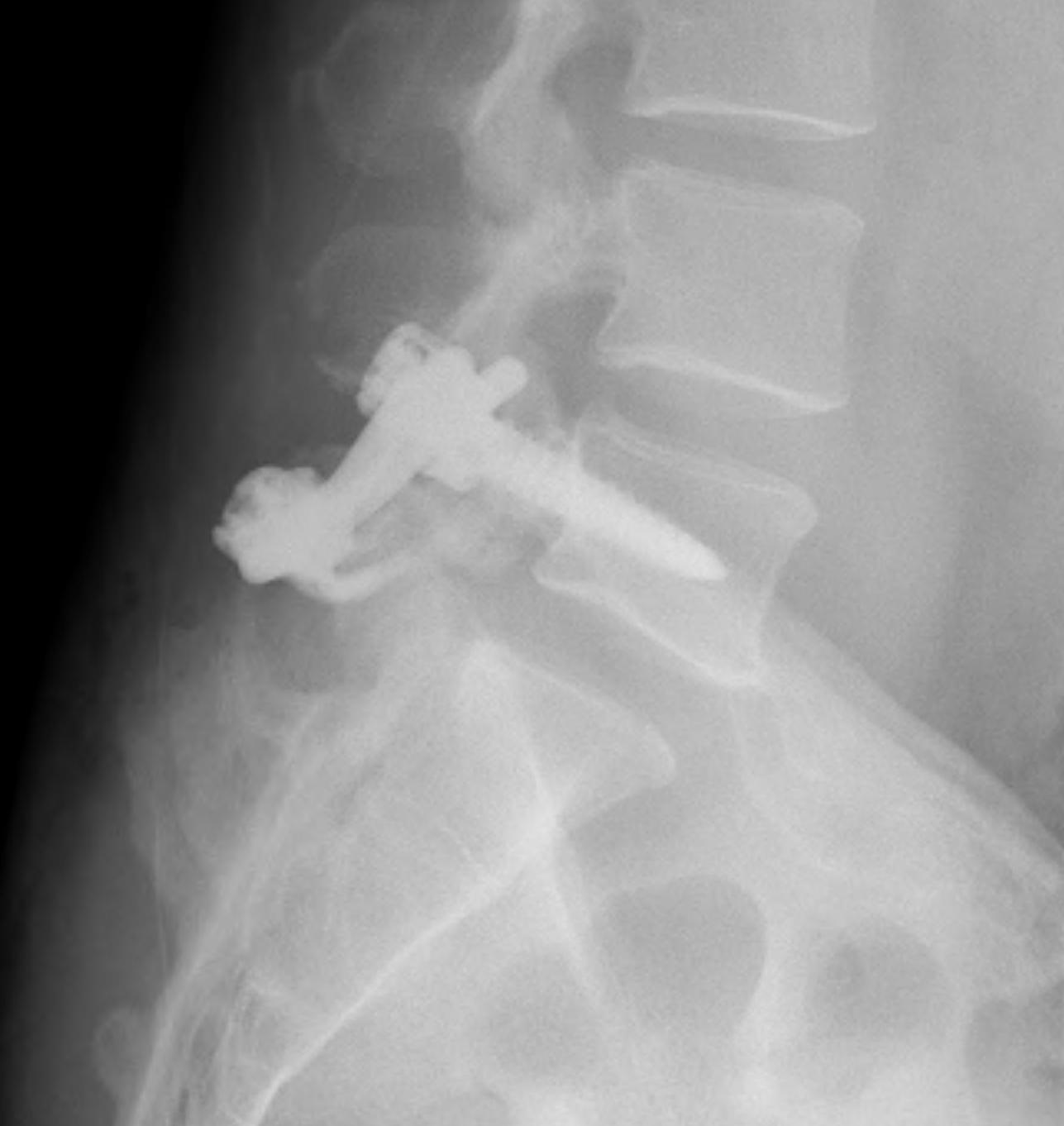
2. Fusion
A. In situ v reduction
- not required for grade 1 - 2
- consider if sagittal malalignment
- associated with risk neurology especially L5
- controversial if should be performed in high grade slips
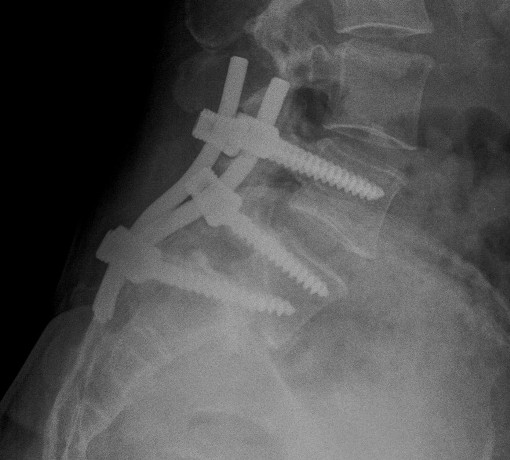
B. Instrumented / non instrumented
C. Levels
- L5/S1 if grade I or II / 50% or less
- L4/S1 if 50% for more
D. Interbody cages
- useful in long standing spondylolithesis presenting in adulthood
- degenerative disc disease
- nerve root pain from interforaminal compression
- improves nerve root space
- improves healing rate
E. Posterior v circumferential
- circumferential approaches may improve fusion rates and outcome in high grade slips
Fusion of Pars
Indication
- normal discs and facets
- pain relieved by pars injection
- failure brace / non operative treatment
- minimal slip

Technique
- lesion identified / debrided / iliac crest bone graft
Options ORIF
1. Screw across lytic defect
- unilateral defect




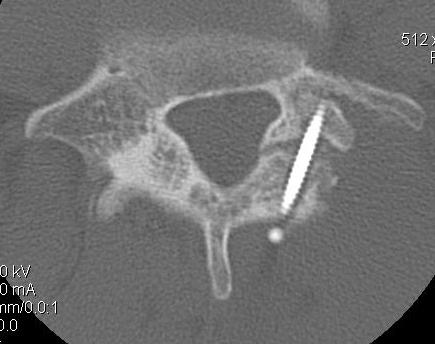
2. Pedicle screw + laminar hook
- bilateral defect



3. TBW spinous process and transverse process
Results
Kakluchi et al JBJS Am 1997
- 16 patients with failure non operative treatment bilateral pars defect
- pain relieved by pars injection with LA
- pedicle screw + lamina hook
- nerve root decompression where required
- union in all 16
- 3 patients only had occasional back pain
Fusion in Situ
A. Wiltse Lateral Mass Fusion in situ
Concept
- in situ fusion via a paraspinal muscle splitting approach
- no reduction or instrumentation
Indication
- for L5/S1 with minor slip in young patient
- rarely done these days
- most surgeons perform instrumented fusion
Technique
- midline incision
- two paramedian incisions in lumbodorsal fascia 4.5cm lateral to midline
- paraspinous muscle splitting approach 2 fingerbreadths lateral to midline
- split sacrospinalis using finger to dissect through muscle
- don't go anterior to TP or risk damage to nerve root
- decorticate TP / Sacral ala / facet / famina and add crest graft / allograft / BMP
Post-op
- spica 3/12 with 1 leg incorporated
- activity modification for 6/12
Instrumented fusion in situ without reduction
Indications
- slip grade 1 or II
- grade III or IV with no sagittal malalignment
Levels instrumentation
- L5 / S1 grade I or II
- L4 / S1 grade III or IV
Options
1. Pedicle screw instrumentation

2. PLIF / interbody cage

3. Bohlman procedure
- interbody fusion with fibula strut
- augmented with decompression and PLF

4. Transfixing L5 / sacral screw

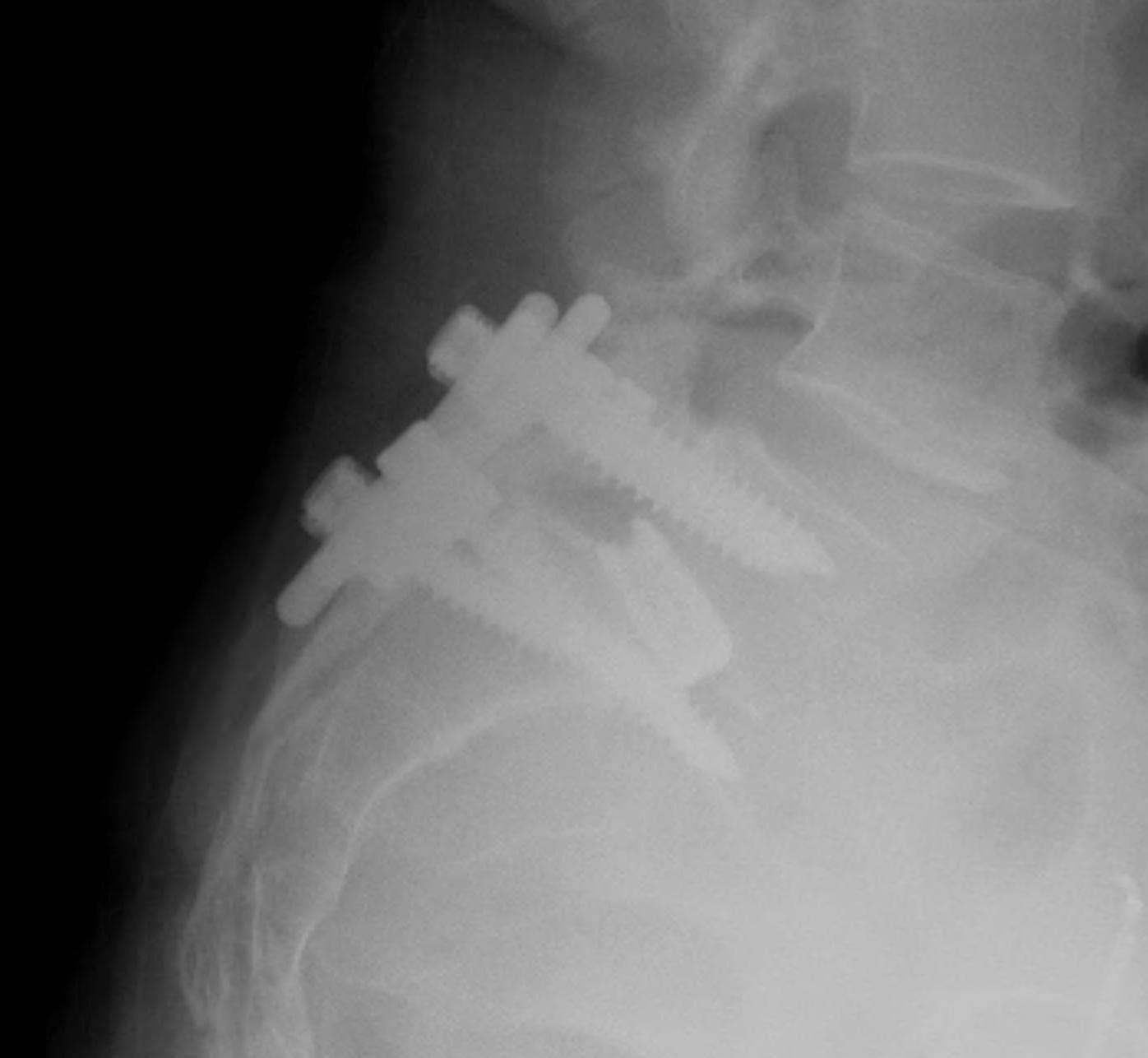
Reduction + Instrumented fusion
Indications
- sagittal malignment
Disadvantage
- risk of neurology (L5)
- up to 25%, usually transient
Advantage
- cosmesis
- less pain from correction of alignment
- more likely fusion, less pseuodoarthrosis
- improved neurological decompression
Technique
A. Posterior approach
- wide foraminatomy bilateral to protect L5 nerve root
- disc removed
- screws used to correct angulation +/- some translation
- interbody fusion device to restore height
B. Anterior approach
Spondyloptosis
Option
A. L5 vertebrectomy / Gaines procedure
B. Reduction and fusion as above
